L. M. Kodadek1, W. Jiang2, C. K. Zogg2, S. R. Lipsitz2, J. S. Weissman2, Z. Cooper2, A. Salim2, S. L. Nitzschke2, L. L. Nguyen2, L. A. Helmchen3, L. Kimsey4, S. T. Olaiya4, P. A. Learn4, A. H. Haider2 3George Mason University,Department Of Health Administration And Policy,Fairfax, VA, USA 4Uniformed Services University Of The Health Sciences,Bethesda, MD, USA 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA 2Brigham And Women’s Hospital,Center For Surgery And Public Health,Boston, MA, USA
Introduction: Race and insurance status are both independent predictors of outcome disparities after traumatic injury, but it remains unclear whether universal insurance may attenuate racial disparities. We investigated for the presence of racial disparities in a cohort of adult trauma patients with TRICARE coverage (military health system insurance).
Methods: We identified patients (age ≥18), including uniformed service personnel, dependents and retirees, who were treated in the United States for non-combat index injuries between 2006 and 2010. Included patients had a primary diagnosis of traumatic injury (ICD-9 800-959.9) and an Injury Severity Score (ISS) ≥9. Patients with superficial injuries, foreign body injuries and late effects were excluded. Patient demographics as well as clinical and hospital characteristics were compared by race. Multilevel logistic regression, adjusting for potential confounding and accounting for clustering of patients within hospitals, determined whether race is an independent predictor of mortality, major morbidity or readmission following traumatic injury among patients with universal insurance coverage. Interaction between trauma outcomes by race and hospital type (civilian or military) was tested.
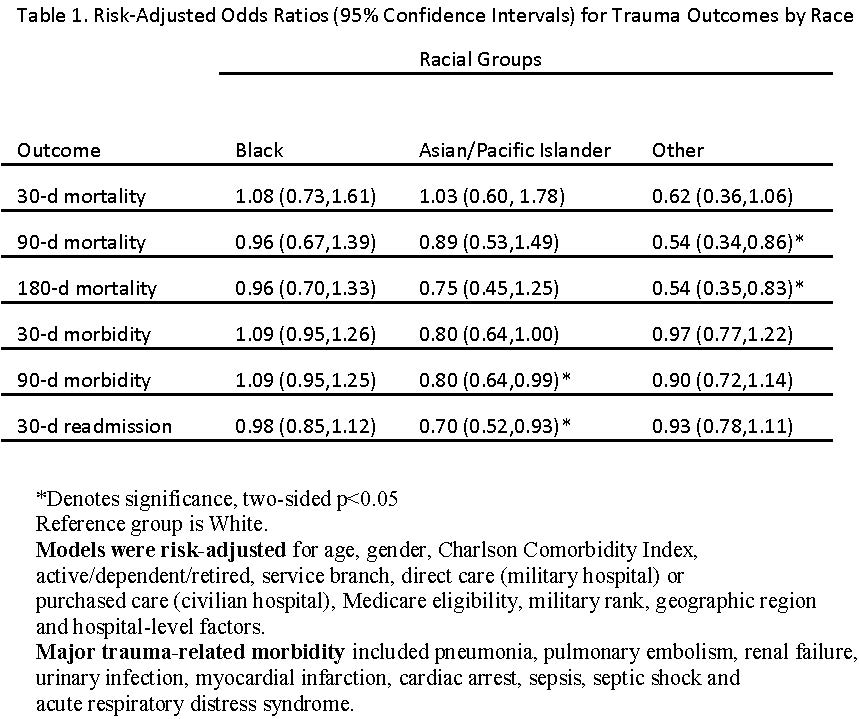
Results: Identified trauma patients (N=19,024) were young (58% of patients age <35), predominantly male (76%) and healthy (89% of patients had Charlson Comorbidity Index = 0); 77% were White, 13% Black and 5% Asian/Pacific Islander. The remaining 5% identified with other races. The largest proportion of patients was active duty or guard (64%) and received care at a civilian hospital (63%). Compared to White patients, minority patients admitted for primary trauma did not experience worse outcomes with respect to morbidity, mortality or readmission. Some groups experienced better outcomes than White patients: Asians/Pacific Islanders had significantly lower odds ratios of 90+ day morbidity and 30+ day readmission, while patients of minority races other than Black and Asian/Pacific Islander experienced lower mortality at 90 and 180 days. There was no significant interaction between race and hospital type (civilian versus military). Risk-adjusted regression results are presented in Table 1.
Conclusion: Universal military insurance coverage was associated with resolution of racial disparities in morbidity, mortality and readmission after traumatic injury. While unmeasured confounders, including socioeconomic status, may limit direct comparison with an injured civilian population, these findings highlight a role for universal insurance coverage for traumatic injury to mitigate known racial disparities in outcomes.