W. A. Marshall1, A. J. Tector1, T. C. Borup1, R. S. Mangus1 1Indiana University School Of Medicine,Surgery/Transplant,Indianapolis, IN, USA
Introduction:
Flushing of the biliary microvasculature at the time of whole organ liver graft procurement appears to be an important component in optimizing blood flow to the biliary system. Two primary preservation solutions are most commonly employed in the United States, University of Wisconsin (UW) and Histidine-Tryptophan-Ketoglutarate (HTK) solutions. While HTK has a viscosity similar to that of water, UW is much more viscous. It has therefore been proposed that the less viscous HTK provides a better flush of the liver graft at the time of procurement. This then leads to the question of whether or not this improved flush results in a lower rate of biliary complications in HTK preserved livers, particularly donation after circulatory death (DCD) grafts. The present study evaluates biliary complications in 1527 consecutive liver transplant patients. The primary study variable is the choice of graft preservation solution, UW or HTK. Outcomes include post-transplant biliary complications, as well as graft and patient survival. Measured biliary complications include any need for bile duct imaging, intra- and extra-hepatic stricture formation, and bile duct leak. The secondary outcome was graft survival.
Methods:
Data were extracted retrospectively from a large, single center database covering the period from 2001 to 2014. All primary imaging reports were reviewed. For this study, a patient was considered to have an anastomotic stricture if this is reported, and an intervention (balloon dilation or stent placement) is performed. Patients in whom sphincterotomy alone was performed were not considered to have a stricture. Any leakage of contrast from the biliary system was considered a biliary leak, though most were easily managed with temporary stenting of the duct.
Results:
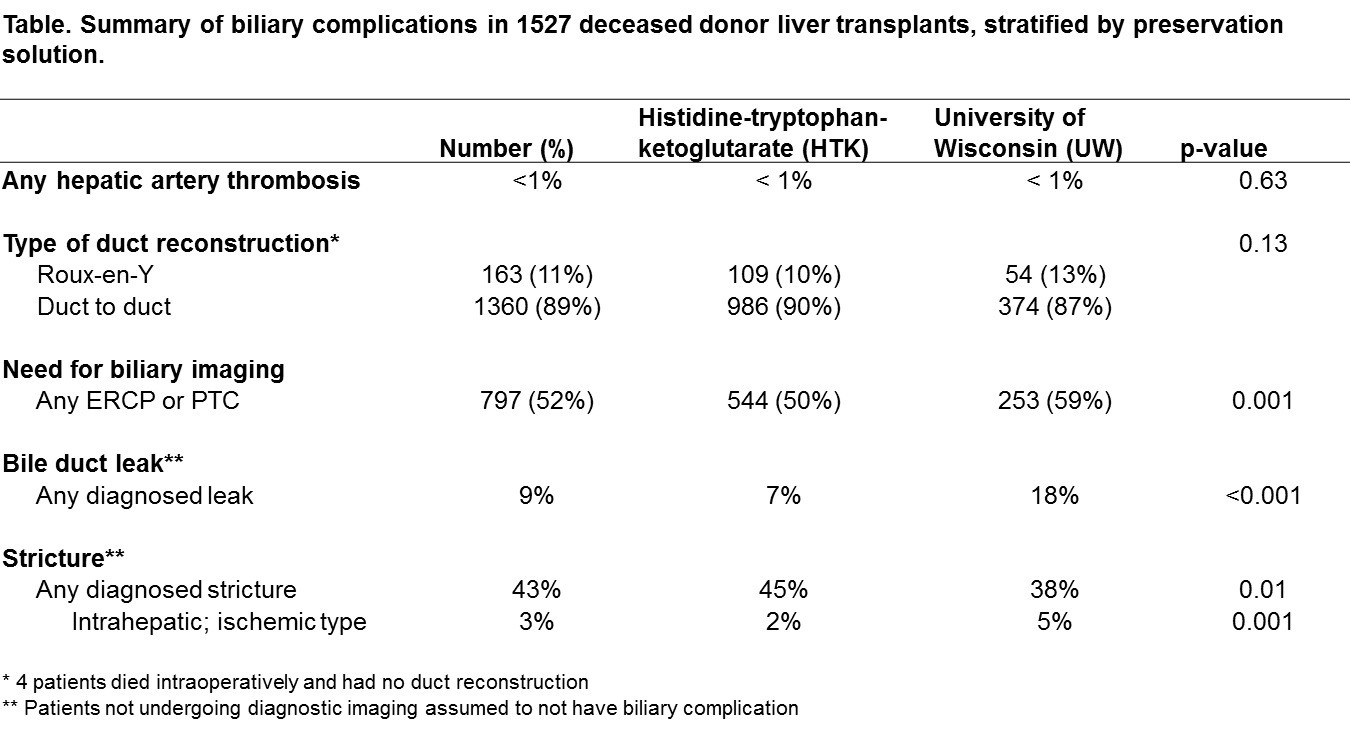
There were 1527 LTs reviewed, 1360 (89%) with duct-to-duct and 163 (11%) with Roux-Y choledochojejunostomy. Preservation included 1098 HTK (72%) and 429 UW (28%) grafts. One-year graft survival favored HTK preserved livers (88% vs 84%, p=0.02). Any biliary imaging was required for 50% of HTK and 59% of UW LTs (p=0.001). The risk of any leak was higher for UW (18%) versus HTK (7%) (p<0.001). The risk of any stricture was higher for HTK (45% vs 38%, p=0.01), but intrahepatic strictures were more common for UW (5% vs 2%, p=0.001). Among donation after circulatory death (DCD) grafts, there was a higher risk of intrahepatic ischemic-type strictures in UW-preserved grafts (36% vs 8%, p=0.02). Survival at 10-years favored HTK.
Conclusion:
HTK liver graft preservation in deceased donors is associated with better graft survival, less imaging, less risk of biliary leak and intrahepatic stricture, and a lower risk of intrahepatic strictures in DCD grafts.