J. G. Wiener1, L. Goss1,2, D. I. Chu1, J. S. Richman1, J. A. Cannon1, T. S. Wahl1, G. D. Kennedy1, K. D. Cofer1, P. K. Patel1, M. S. Morris1 2Birmingham VA Medical Center,Surgery,Birmingham, ALABAMA, USA 1University Of Alabama at Birmingham,Surgery,Birmingham, Alabama, USA
Introduction:
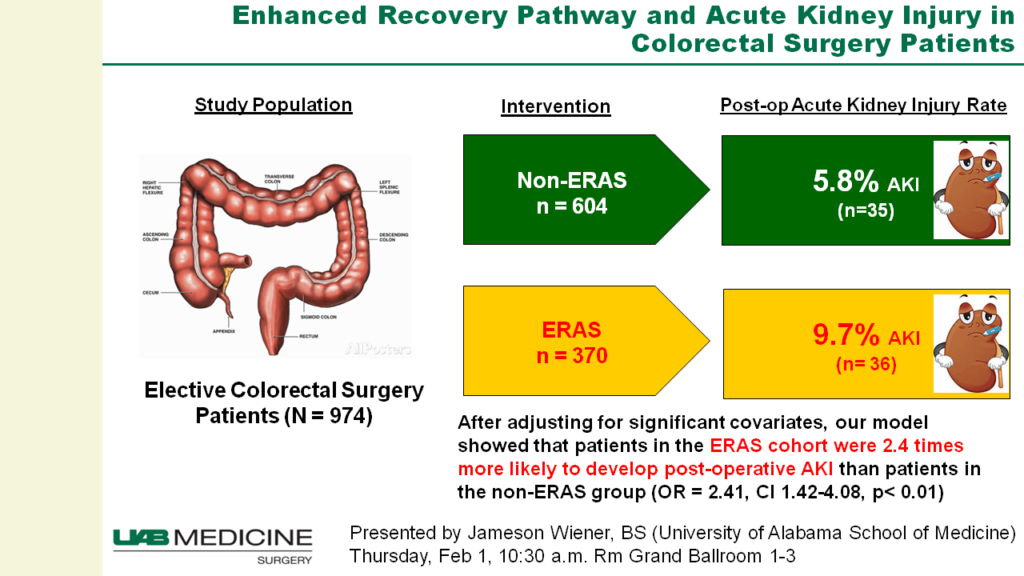
Enhanced Recovery After Surgery (ERAS) pathways standardize preoperative, intraoperative, and postoperative care including goal directed fluid administration and multimodal pain management. ERAS is associated with shorter hospital lengths of stay, lower costs, and equivalent readmission rates. Since implementing ERAS at our institution in 2015, we sensed an increase in AKI. Although ERAS has benefits for patients and hospitals, little is known about its association with acute kidney injury (AKI). We hypothesize that incorporation of an ERAS pathway for elective colorectal surgery would be independently associated with an increased risk of AKI.
Methods:
A single-institution retrospective review of patients undergoing elective colorectal surgery before and after the implementation of ERAS was conducted. Patient-specific variables were recorded and our primary outcome was development of an AKI. AKI was operationalized using The Kidney Disease: Improving Global Outcomes (KDIGO) definition and staging system. Patients with AKI or dialysis preoperatively were excluded from our analysis. Bivariate comparisons were made using chi-square and Wilcoxon rank sum tests for categorical and continuous variables, respectively. Variables with p<0.05 for bivariate comparisons were included in a multivariate logistic model for AKI.
Results:
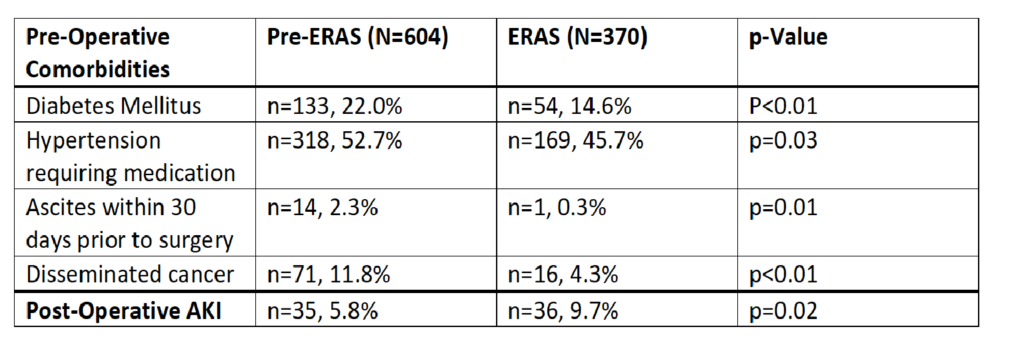
Our study cohort included 974 total patients, 604 in the pre-ERAS group and 370 patients in the ERAS group. The two groups were similar except for significantly higher incidences in the pre-ERAS group of diabetes mellitus, hypertension requiring medication, ascites within 30 days prior to surgery, disseminated cancer, and contaminated or dirty wounds in the pre-ERAS group compared to the ERAS group (Table). There was no significant difference in age or BMI at the time of surgery between the two groups. Postoperatively, 9.7% of the ERAS group developed AKI compared to 5.8% of the pre-ERAS group (p=0.02). After adjusting for significant covariates, our model showed that patients in the ERAS group were 2.4 times more likely to develop post-op AKI than patients in the pre-ERAS group (OR=2.41, CI 1.42-4.08, p < 0.01).
Conclusion:
Implementation of an Enhanced Recovery Protocol is associated with higher levels of acute kidney injury following elective colorectal surgery. Future studies will determine which aspects of the ERAS protocol, such as NSAID use in the multi-modal pain management or intraoperative goal directed fluid delivery, may be associated with this increased incidence of AKI.