A. Lai1, D. Kim1, C. Kapsalis1, D. Ciesla1 1University Of South Florida College Of Medicine,Tampa, FL, USA
Introduction:
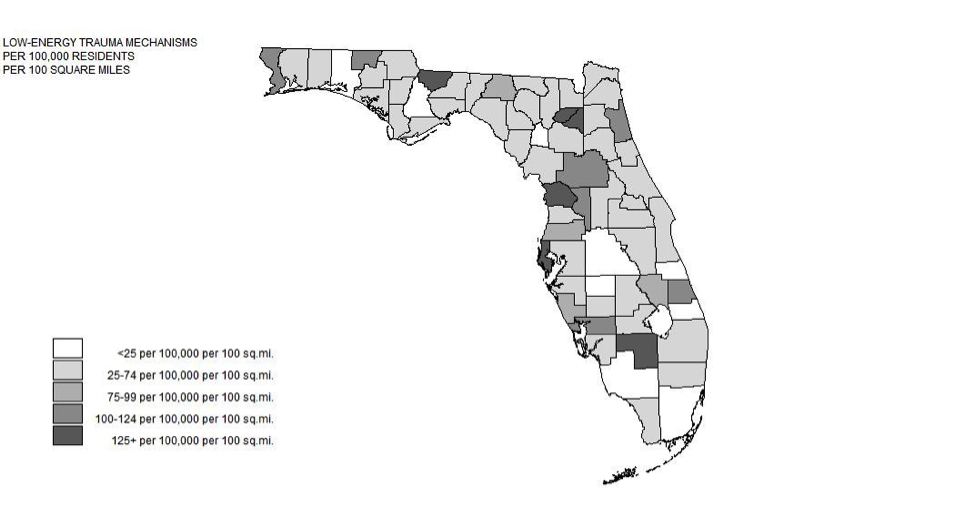
Traumatic injuries are the third leading cause of mortality amongst Americans. Injury mechanisms can be separated into individual events (e.g. falls) or interaction events (e.g. motor-vehicle accidents). Interaction events occur between individuals and are expected to be higher amongst regions with higher population density. We aimed to see whether collisions mechanisms in Florida counties increased with population density.
Methods:
Data for this retrospective cohort study were obtained from the 2013 Florida Agency for Healthcare Administration (AHCA) discharge database. All patients with trauma alert charges or admission type defined as trauma were included. Additionally, any admissions classified as urgent or emergent with any ICD-9 codes between 800 and 957 were included. Patients were excluded if they were pronounced dead on arrival. County populations were taken from the 2013 Census Data estimates, and county-level characteristics were taken from 2010 Census Data estimates.
Results:
Age-adjusted population density was not a significant predictor of low-energy mechanisms (p=0.1063); however, median county age was a significant predictor in the model (p=0.0340). The model was a significant (p=0.0173). Age-adjusted population density was not a significant predictor of high-energy mechanisms (p=0.8271). Median age was not a significant predictor (p=0.8218), and the model was not significant (0.9433).
Conclusion:
Both low-energy and high-energy mechanisms do not appear to be linearly correlated with population density after adjustment for median county age. The data suggest that both trauma mechanisms appear to occur independent of population density in Florida.