J. Rosado2, J. B. Oliver2, J. Patel2, K. M. Spiegler2, K. Houck3, R. J. Chokshi1 1New Jersey Medical School,Surgical Oncology,Newark, NJ, USA 2New Jersey Medical School,Surgery,Newark, NJ, USA 3New Jersey Medical School,Obstetrics And Gynecology,Newark, NJ, USA
Introduction: Cytoreduction surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) offer the best opportunity for long term survival for peritoneal metastasis for colorectal, appendicular, and ovarian cancers. There are times in which to achieve proper cytoreduction, abdominal wall resection is required. These resections in part the need for abdominal wall reconstruction while some patients require reconstruction for other reasons as well. It is known that chemotherapy and hyperthermia in part increased risks for wound infections, poor wound healing and further complications. Therefore, we looked at the outcomes in our series of CRS-HIPEC patients taking a look at the outcoomes, morbidity and mortality of those patients requiring abdominal wall reconstruction compared to those who did not.
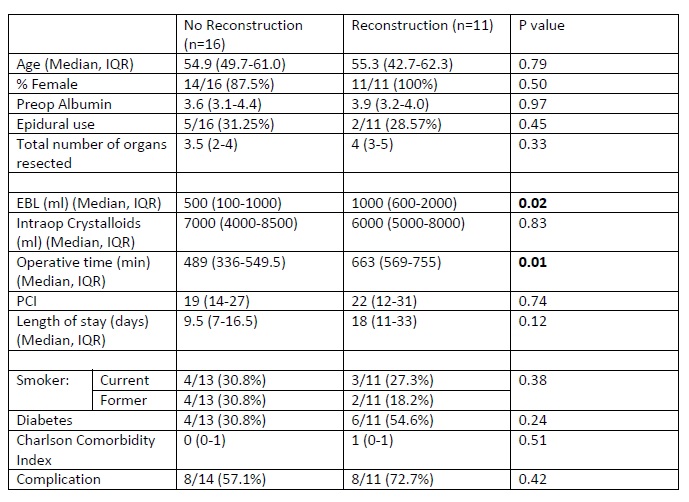
Methods: Demographics, comorbidities, intraoperative variables, and post-operative outcomes for all patients undergoing CRS/HIPEC at a single institution from 2012 to 2015 were analyzed. Variables were examined with chi squared or Wilcoxon Ranked Sum Test where appropriate. Survival was analyzed with Kaplan Meier curves and Cox Proportional Hazards Regression..
Results:During this time frame, 27 individuals underwent CRS-HIPEC. There were 11 patients which underwent reconstruction, while 16 patients had no reconstruction. These patients were similarly aged and gender distribution. They had similar epidural use and similar number of organs removed. There was no difference in Peritoneal Carcinomatosis Index for the two groups (22 vs 19 p=0.74). Patients undergoing reconstruction tended to have increased operative time (663min vs 489min p=0.01) as well as increased blood loss (1000ml vs 500ml p=0.02). Both groups had similar complication rate (72.7% vs 57.1% p=0.42). Median follow up for the no reconstruction group was 4 months compared to 1.7 months for the reconstruction group. Five of the 16 individuals within the no reconstruction group and 3 of the 11 individuals with reconstruction died during the follow up period. The survival rate for the two groups were similar (68.8% vs 72.7%, p=0.44).
Conclusion:Thus the need for abdominal wall reconstruction had no impact on patient’s mortality but did impact their operative time and blood loss. Further evaluation with larger series and longer follow up is needed to confirm these findings.