K. Kniery1, M. DeHart1, S. Salgar1 1Madigan Army Medical Center,Clinical Investigation,Tacoma, WA, USA
Introduction:
During the global war on terrorism (2001-2008) in Iraq and Afghanistan, 737 US military service members sustained major limb amputations. Limb transplantation offers hope to improve the quality of life. We investigated whether mesenchymal stem cell (MSC) and G-CSF therapy can improve functional recovery in nerve transection-repair and limb transplant models.
Methods:
Under general anesthesia the sciatic nerve branches (tibial, peroneal and sural) were transected and repaired. In another group, syngeneic right hind limb transplantation was performed. MSCs (5×106; passage ≤6), G-CSF (50µg/kg), or Vehicle were administered topically and i.v./i.p.
Results:
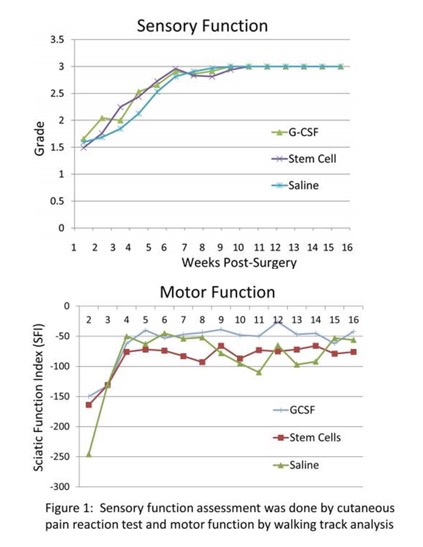
At two weeks post-nerve repair, sensory function (SF) in all groups was ~1.5 on a scale of Grade 0-3 (0=No function; 3=Normal function). By 4 weeks it was 2.2±1.0, 2.0±1.2, and 1.8±1.3 in MSC, G-CSF and Vehicle treated groups, respectively. By 10 weeks, normal SF (~3) was restored in all groups (n=8/group). The sciatic nerve function index (SFI) a measure of motor function (0=normal; -100 =nonfunctional) during 5-16 weeks was markedly improved in G-CSF (-40 to -26) compared to MSC (-93 to -66) or Vehicle (-110 to -45) group (Figure1). In limb transplants, SF recovery ranged 0.8-1.3 by 8 weeks, and 1.5-2.0 by 16 weeks post-surgery. Limb transplants (~60%) developed flexion-contractures and we were unable to calculate SFI. Fewer animals in G-CSF (37%) compared to Vehicle (66%) group developed contractures. Gastrocnemius muscle atrophy was evident in limb transplants.
Conclusion:
G-CSF and MSC therapies appear to promote sensory and motor function recovery in nerve transection-repair and limb transplant models.