K. A. Kelley1, R. Ruhl3, S. Rana2, C. R. Thomas2, S. Anand2,3, V. L. Tsikitis1 1Oregon Health And Sciences University,Department Of Surgery,Portland, OREGON, USA 2Oregon Health And Sciences University,Department Of Radiation Medicine,Portland, OREGON, USA 3Oregon Health And Sciences University,Department Of Cell, Developmental, Cancer Biology,Portland, OREGON, USA
Introduction:
Chemoradiotherapy (CRT) response is an independent predictor of overall survival in locally advanced rectal cancer, highlighting the importance of improving CRT response rates. It is known that several tumor intrinsic factors govern responses to radiation therapy. Emerging evidence suggests that microRNAs (miRs) modulate gene expression profiles in response to radiation.
Methods:
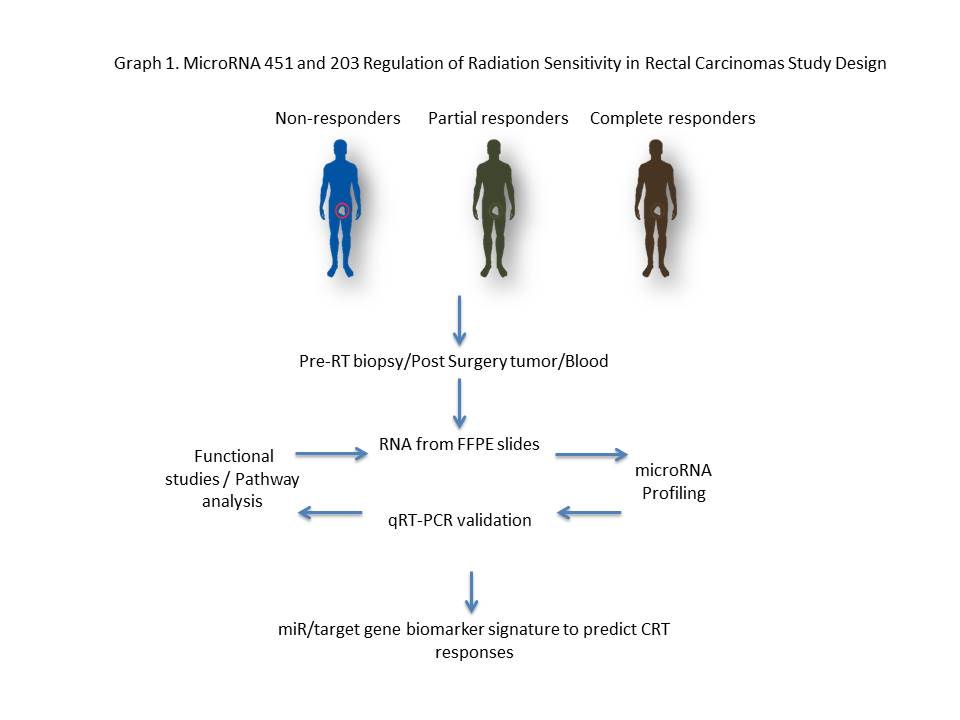
microRNA profiles were examined and analyzed in approximately forty rectal cancer patients that had either a pathological partial response (PR) or no response (NR). Using Nanostring technology, a miR profiling platform, miRNAs significantly down and up regulated were identified in FFPE biopsy specimens. mRNA differentially expressed was followed by in vitro radiation models and tumor sphere assays. Graph 1.
Results:
miR-451a was among the most upregulated miRs in the PR group whereas miR-203 was among the most downregulated miR. Inhibition of miR-451a in HCT-116 significantly increased survival in response to a 2 Gy dose of radiation; conversely, transfection of a miR-451 mimic significantly decreased cell survival, with more than a 12-fold decrease when combined with a 5 Gy dose fraction. Consistent with these results, miR-451a inhibition increased proliferation in 2D as well as in a tumor sphere assay, whereas transfections of a miR-451a mimic robustly decreased proliferation. In contrast to miR-451a, miR-203 was downregulated in patients with a partial response to CRT. Inhibition of miR-203 increased apoptosis in combination with a 5 Gy dose fraction.
Conclusion:
A gain of miR-451a and an inhibition of miR-203 in tumor cell lines enhanced cell death and decreased survival in combination with radiation. In this context, we hypothesize that differential expression of miRs regulates rectal cancer radiation sensitivity and therefore can be used as a biomarker to predict therapeutic responses to radiation therapy.