A. Nayyar1, S. Scarlet1, P. D. Strassle1, D. W. Ollila1, L. M. Erdahl3, K. P. McGuire2, K. K. Gallagher1 1University Of North Carolina At Chapel Hill,Department Of Surgery,Chapel Hill, NC, USA 2Virginia Commonwealth University,Department Of Surgery,Richmond, VA, USA 3University Of Iowa,Department Of Surgery,Iowa City, IA, USA
Introduction:
Emerging data suggests that experiencing sexual harassment in the workplace is a common occurrence for women across all professions, which can be harmful personally and professionally. While recent studies have reported the incidence of sexual harassment in medicine, no study has examined the nature or scope of sexual harassment experienced by surgeons.
Methods:
An anonymous, electronic survey was distributed via a web-based platform to members of American College of Surgeons (ACS), Association of Women Surgeons (AWS), and through targeted social media platforms from April-July 2018. Questions pertained to workplace experiences and frequency of sexual harassment in the past 12 months. Sexual harassment was defined according to the U.S. Equal Employment Opportunity Commission. Fisher’s exact and Mantel-Haenszel tests were used to assess differences in respondent characteristics.
Results:
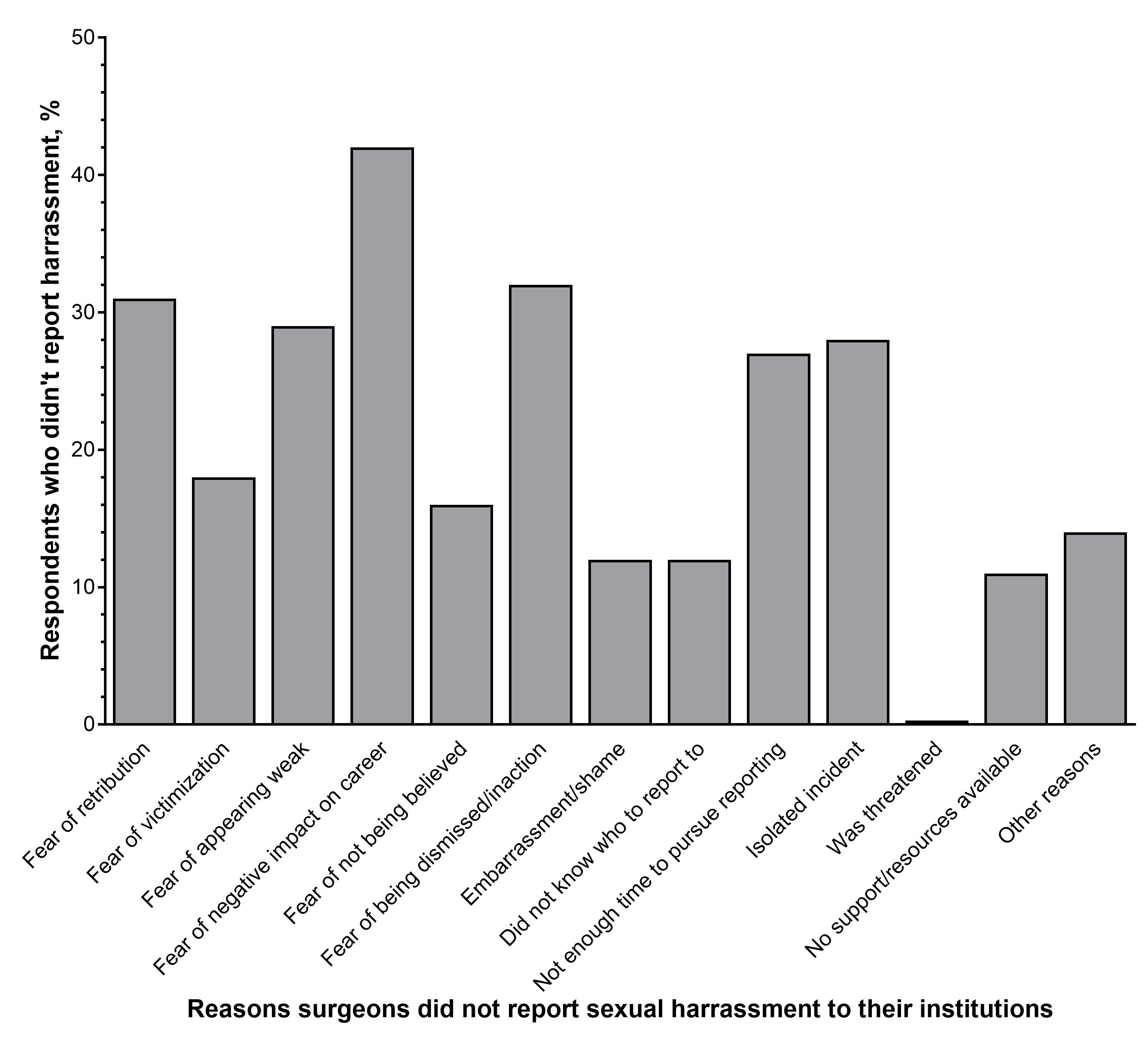
1,005 individuals completed the survey. 74% (n=744) identified as women, a response rate of 18% among US women surgeons. 25% (n=249) of respondents identified as men which represents 1% of male surgeons in the US – these responses were analyzed separately. Respondents reported employment by an academic institution (51%), community medical center (13%), private practice (15%), or other (19%). For both genders, the most common specialties were general surgery (34%), trauma surgery (10%), and surgical oncology (8%). Overall, 58% (n=432) of women surgeons experienced sexual harassment within the 12-month period preceding the survey, compared to 25% (n=61) of men, p<0.0001. Among women, the most common forms of harassment reported were “verbal or physical conduct (e.g. body language)” (53%), “unwanted sexual advances or physical contact” (23%), and “comments about sexual orientation” (10%). Women trainees were more than twice as likely to experience harassment as compared to attending surgeons (OR 2.52, 95% CI 1.78, 3.56, p<0.0001). The majority (84%) of incidents of harassment reported by women as part of the survey were not reported to any institutional authority. The most common reasons for not reporting was “fear of a negative impact on my career” (43%), “fear of retribution” (32%), and “fear of being dismissed and/or inaction towards perpetrator” (31%) (Figure).
Conclusion:
Our study indicates that there is an alarming prevalence of unreported sexual harassment experienced by women surgeons in the US. Combined with the documented sexual harassment of women physicians in other medical specialties, we believe this finding demonstrates an urgent need to improve the safety of the healthcare workplace, not just for women surgeons, but for all.