E. Dobrinskikh1, S. I. Al-Juboori2, U. Shabeka2, A. I. Marwan2 1University Of Colorado Denver,Medicine,Aurora, CO, USA 2University Of Colorado Denver,Division Of Pediatric Surgery, Department Of Surgery,Aurora, CO, USA
Introduction: The mammalian respiratory system is a highly specialized organ. The bidirectional interactions between endoderm and the surrounding mesoderm are important for coordinated differentiation of the respiratory epithelial cells, and the formation of vascular capillary network with a common basement membrane, which is crucial for gas exchange. Basement membrane components play a dynamic role as a barrier and reservoir for different growth factors. Proper expression and function of the basement membrane extracellular matrix (ECM) are necessary for normal lung growth and development. However, little is known how the proliferative state of the alveolar epithelial cells (AEC) can influence ECM composition. Previously we have shown that tracheal occlusion, an experimental therapeutic intervention used to induce lung growth, in normal lungs leads to the formation of at least two zones; with control-like signatures and zones with enlarged airspaces and a metabolic shift to glycolysis, which could indicate a presence of proliferating cells. Thus, in this study we tested the hypothesis that in zones with enlarged airspaces, type 2 AEC are shifted towards proliferation and therefore can lead to a change in the surrounding ECM composition.
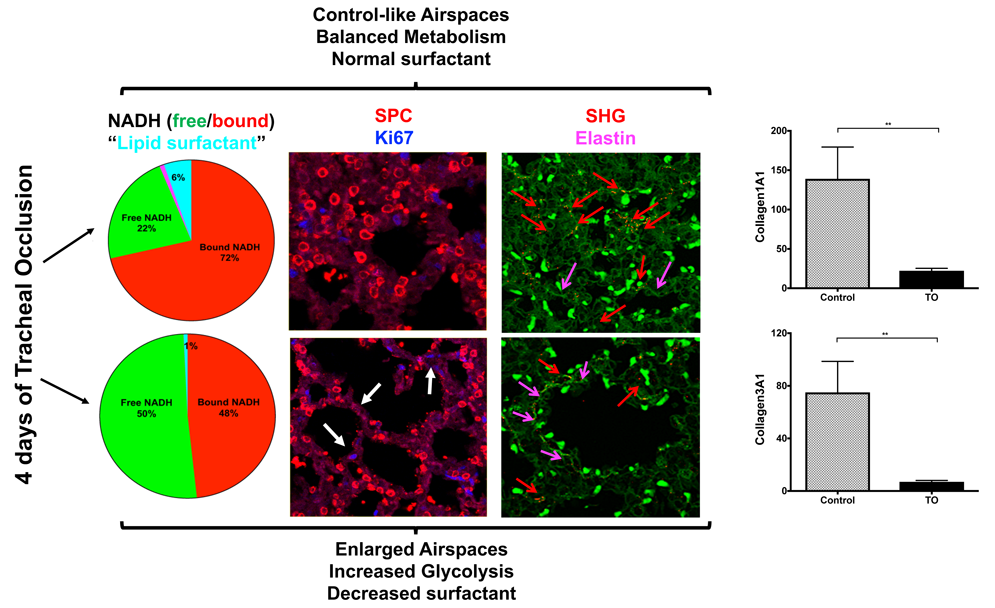
Methods: RNAScope combined with immunofluorescence (IF), global proteomics, Fluorescence Lifetime Imaging Microscopy (FLIM), Second harmonic generation (SHG) imaging analyses were used to characterize control-like and enlarged airspaces in normal fetal rabbit lungs following 4 days of tracheal occlusion. Tissues were harvested at 30 days of gestation.
Results: RNAScope for SPC or SPA mRNA expression, in a combination with IF for proSPC protein and proliferation marker (Ki67), revealed almost absent double-positive AEC2 in control-like airspaces at this gestational age, whereas in the enlarged airspaces an increase in proliferating AEC2 was observed. Global proteomics of a whole lung lobe revealed a significant decrease in multiple ECM components; including collagen 4 (a major component of the basement membrane) in addition to collagens 1 and 3 (main structural collagens of different connective tissues, including parenchymal vasculature). FLIM showed that in the zones with a shift toward glycolysis and enlarged structures there was an appearance of a strong signal, corresponding to elastin lifetime. SHG confirmed increased signal for elastin in addition to a decrease of fibrillar collagens 1 and 3 nearby big airspaces.
Conclusion: For the first time we have shown that heterogeneous parenchymal changes following 4 days of tracheal occlusion are accompanied by changes in ECM components composition. These changes are correlated with increased number of proliferating AEC2 cells.