C. J. Pokrzywa1, C. M. Papageorge2, L. Durbak2, G. D. Kennedy2 1University Of Wisconsin,School Of Medicine And Public Health,Madison, WI, USA 2University Of Wisconsin,General Surgery,Madison, WI, USA
Introduction: It has been suggested in the orthopedic surgery literature that preoperative urinary tract infection (UTI) may be associated with surgical site infections secondary to hematogenous spread of bacteria. However, association between preoperative UTI and postoperative complications has not been evaluated in general surgery populations. We hypothesized that UTI present at the time of surgery is associated with higher incidence of short-term postoperative morbidity in patients undergoing elective general surgery.
Methods: Patients undergoing elective general surgical procedures from 2011-2013 were selected from the national American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) participant use file. Exclusion criteria included emergent procedures, ASA class 5 or unknown, preoperative ventilator-dependence, SIRS, sepsis, septic shock, and missing preoperative UTI data. Patients were divided into two cohorts based on presence or absence of UTI at the time of surgery and were then matched 1:2 (case:control) on age, ASA class, and primary CPT. Univariate analysis was performed using Chi-squared or Fisher’s exact tests to compare the two cohorts with regards to patient demographics, comorbidities, and postoperative complication rates. Postoperative morbidity was analyzed using multiple logistic regression to control for baseline differences between the two groups.
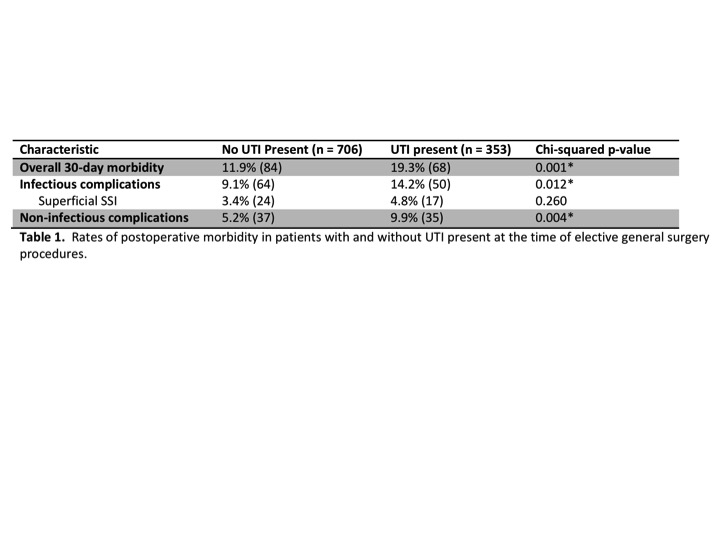
Results: A total of 434,802 patients were identified for inclusion in the study, with an overall preoperative UTI rate of 0.08% (n = 363). After matching, there were 353 patients with UTI and 706 without UTI. The two groups were similar with regards to age, BMI, ASA class, and most comorbidities. There were more females, more Caucasians, fewer Hispanics, more inpatients, and higher frequency of dependent functional status, wound infection, weight loss, and preoperative transfusion in the UTI group. On univariate analysis, the UTI group had a significantly higher incidence of overall morbidity, infectious complications, and non-infectious complications (Table 1). The multivariate analysis confirmed a higher odds ratio of overall postoperative morbidity associated with preoperative UTI when controlling for baseline differences between the two groups (OR 1.504, 95% CI: 1.025-2.207).
Conclusions: We demonstrated an increased rate of 30-day complications in general surgery patients with UTI present at the time of surgery. As surgeons strive to provide safer, higher-quality care, these findings suggest there may be value in attempting to identify and treat UTI preoperatively in patients scheduled for elective general surgery procedures.