J. N. MacTaggart1, W. Poulson1, M. Akhter1, A. Seas1, K. Thorson1, N. Phillips1, A. Desyatova1, A. Kamenskiy1 1University Of Nebraska College Of Medicine,Surgery,Omaha, NE, USA
Introduction:
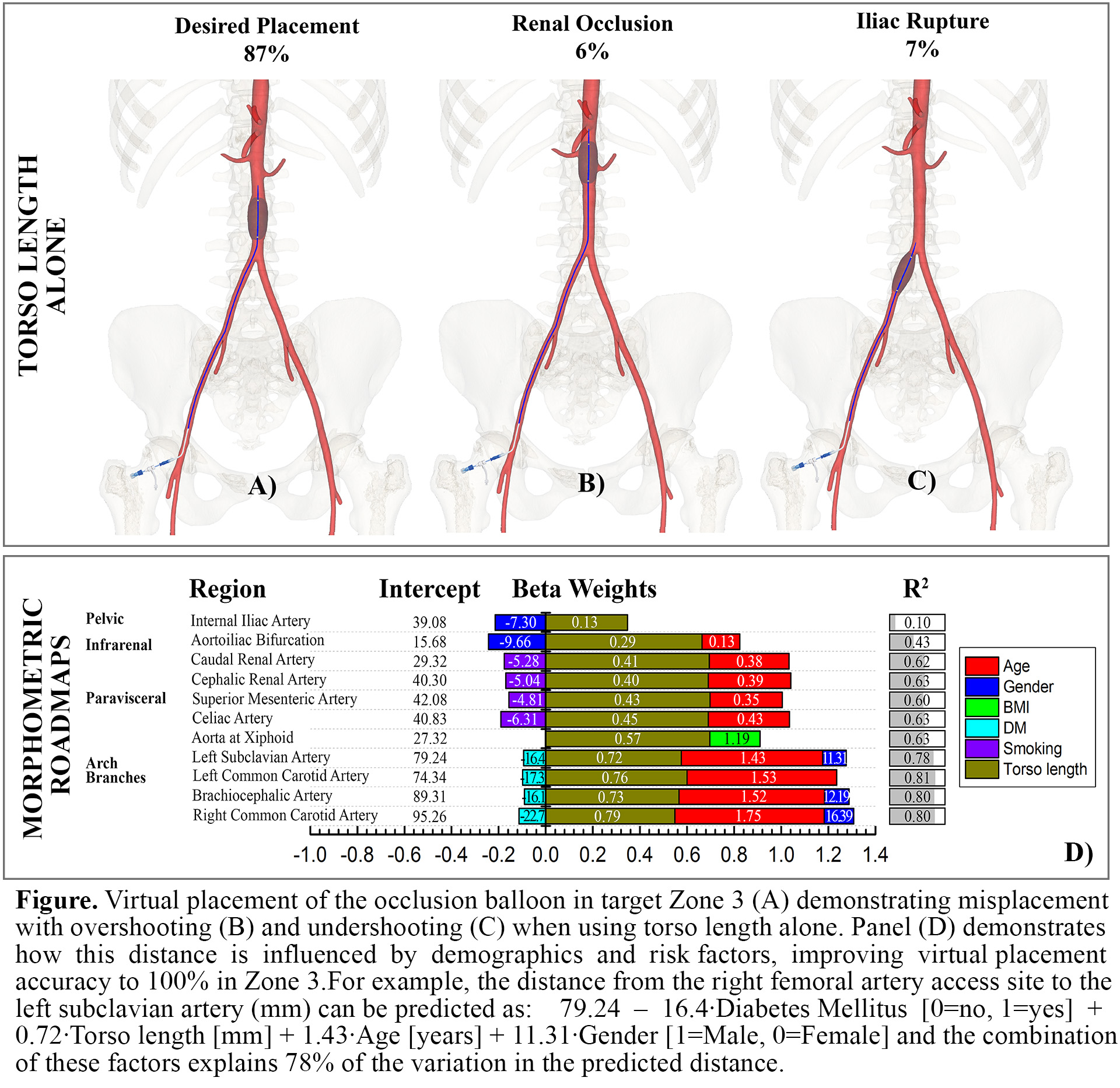
Uncontrolled hemorrhage from large vessel injuries within the torso remains a significant source of prehospital trauma mortality. Resuscitative endovascular balloon occlusion of the aorta can effectively control hemorrhage, but this minimally invasive technique relies heavily upon imaging not available in the field. Our goal was to develop morphometric roadmaps to enhance the safety and accuracy of fluoroscopy-free endovascular navigation of hemorrhage control devices.
Methods:
Three-dimensional reconstructions of thin-section, contrast-enhanced computed tomography angiography scans from n=122 subjects (mean age 47±24 years, range 5-93 years old, 64 Male/58 Female) were used to measure centerline distances from femoral artery access sites to the major aortic branch artery origins. Morphometric roadmaps were created using multiple linear regression analysis to predict distances to the origins of the major arteries in the chest, abdomen and pelvis using torso length, demographics, and risk factors as independent variables. A hypothetical 40-mm long occlusion balloon was then virtually deployed into Zones 1 and 3 of the aorta using these roadmaps, with placement accuracy assessed by comparing predicted versus actual measured distances to the target locations within the aorta.
Results:
Torso length and age were the strongest predictors of centerline distances from femoral artery access sites to the major aortic branch artery origins. Male gender contributed to longer distances to aortic arch branches, while diabetes and smoking history were associated with shorter distances. Hypertension, dyslipidemia and coronary artery disease had no effect. Using morphometric roadmaps, virtual occlusion balloon placement accuracy was 100% for Zone 3 of the aorta, compared to 87% accuracy when using torso length alone (Figure).
Conclusion:
Morphometric roadmaps demonstrate potential for improving the safety and accuracy of fluoroscopy-free aortic occlusion balloon delivery. Continued development and refinement of minimally invasive hemorrhage control techniques could lead to improvements in prehospital mortality for all age groups and both genders of patients with noncompressible torso hemorrhage.