A. I. Salem1, T. B. Tran2, G. A. Poultsides2, S. K. Maithel3, T. S. Wang4, I. Hatzaras5, J. E. Phay6, R. C. Fields7, T. M. Pawlik8, J. D. Prescott8, S. Gad9, A. C. Yopp10, Q. Duh11, C. C. Solorzano12, C. M. Kiernan12, K. I. Votanopoulos13, S. M. Weber1 1University Of Wisconsin School Of Medicine And Public Health,Department Of Surgery,Madison, WI, USA 2Stanford University,Department Of Surgery,Palo Alto, CA, USA 3Emory University School Of Medicine,Department Of Surgery,Atlanta, GA, USA 4Medical College Of Wisconsin,Department Of Surgery,Milwaukee, WI, USA 5New York University School Of Medicine,Department Of Surgery,New York, NY, USA 6Ohio State University,Department Of Surgery,Columbus, OH, USA 7Washington University,Department Of Surgery,St. Louis, MO, USA 8Johns Hopkins University School Of Medicine,Department Of Surgery,Baltimore, MD, USA 9University Of California – San Diego,Department Of Surgery,San Diego, CA, USA 10University Of Texas Southwestern Medical Center,Department Of Surgery,Dallas, TX, USA 11University Of California – San Francisco,Department Of Surgery,San Francisco, CA, USA 12Vanderbilt University Medical Center,Department Of Surgery,Nashville, TN, USA 13Wake Forest University School Of Medicine,Department Of Surgery,Winston-Salem, NC, USA
Background:
The role of laparoscopic resection for adrenocortical carcinoma (ACC) is controversial. Few data are available on surgical outcome and survival benefit. We sought to evaluate the perioperative and long-term outcomes following laparoscopic and open resection of adrenocortical carcinoma.
Methods:
Retrospective data collection of patients who underwent adrenalectomy for pathologically confirmed primary adrenocortical carcinoma in 13 experienced tertiary care cancer centers were analyzed, including demographics, clinicopathological features, and operative outcomes. Outcomes following laparoscopic resection were compared to open resection.
Results:
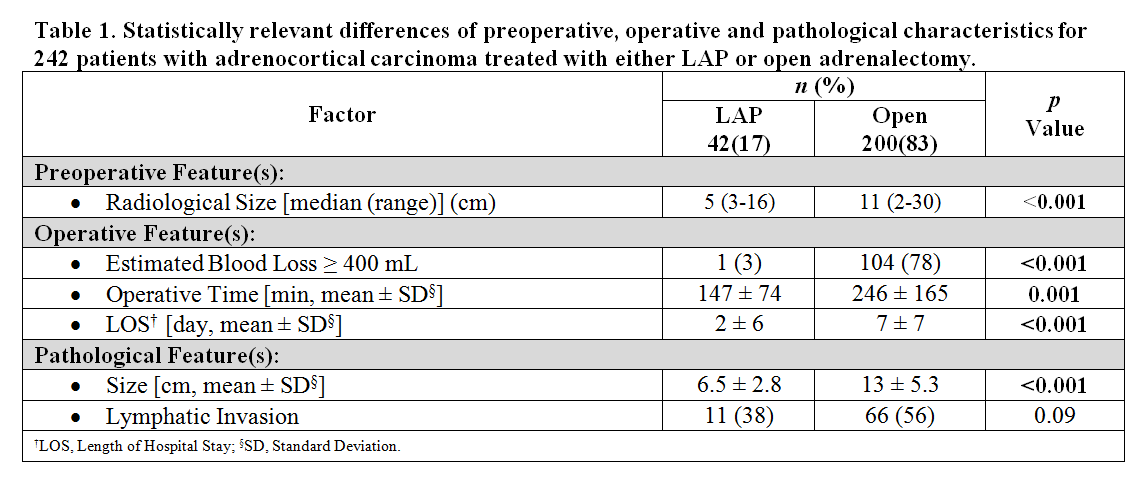
A total of 242 patients were evaluated, including 42 laparoscopic (LAP) and 200 open resections. There was no difference in utilization of LAP approach amongst institutions (p=0.24). There was no difference in in-hospital mortality (0%, LAP vs 2.7%, open, p=0.31) or overall 30-day morbidity (27%, LAP vs 35%, open, p=0.44). The only preoperatively determined predictor of utilization of a LAP approach was radiological size (p<0.001). Of note, utilization of a LAP approach was not associated with tumor laterality, body mass index, or functional tumor status. On univariable analysis, there were a number of perioperative factors associated with utilization of LAP adrenalectomy (Table 1). There was no difference in rates of intraoperative tumor rupture or R0 resection rates. Although there was an association of improved median overall survival in the LAP group on univariable analysis (100 mo. vs 37 mo., p=0.03), after adjusting for age, tumor size, lymphatic invasion and estimated blood loss, there was no difference in overall survival (OR=0.998, p=0.89, CI=0.972 – 1.025).
Conclusion:
Although LAP adrenalectomy was utilized for smaller tumors, there was no association of choice of LAP approach with body mass index, laterality, or functional tumor status. Improvements in perioperative outcomes for LAP cases included estimated blood loss, operative time, and length of hospital stay, without differences in morbidity, mortality, R0 status, or incidence of intraoperative tumor rupture. Randomized controlled trials are needed to confirm the findings of this study.