R. Kashani1, S. Sareh1, M. Tamrat1, N. Satou1, R. Shemin1, P. Benharash1 1David Geffen School Of Medicine, University Of California At Los Angeles,Division Of Cardiac Surgery,Los Angeles, CA, USA
Introduction: Numerous studies have demonstrated the benefits of postoperative aspirin administration following coronary artery bypass grafting (CABG) and other cardiac operations. However, the role of preoperative aspirin administration in cardiac surgery still remains uncertain. While several studies have reported lower mortality rates associated with preoperative aspirin use in CABG patients, there is a paucity of data regarding patients undergoing CABG combined with valvular procedures. The present study aimed to determine the utility of preoperative aspirin administration on clinical outcomes in the setting of combined CABG with valve surgery.
Methods: A total of 565 patients who underwent combined CABG and valve surgery at our institution from 2008 to 2015 were identified for analysis. After exclusion of emergency cases, 536 patients were placed into two groups: those who received aspirin within 5 days prior to surgery (ASA group; n=328), and those who did not (N-ASA group; n=208). Baseline characteristics associated with aspirin use—including age, gender, race, body mass index, recent myocardial infarction, smoking, and use of anticoagulants—were compared between groups. Propensity score matching based on twenty-five preoperative factors was then used to account for intergroup differences. Logistic regression models were developed to compare the rate of postoperative complications, including renal failure, major adverse cardiovascular events (MACE), and 30-day mortality, between groups. All statistical analysis was performed using Stata 13.0 (StataCorp, College Station TX).
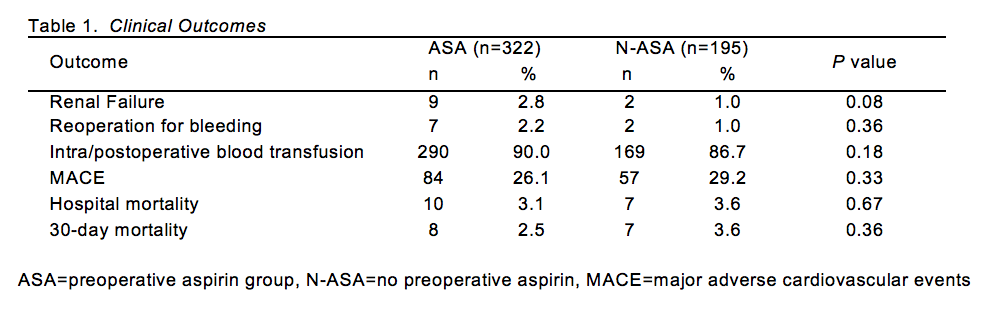
Results: After propensity score matching, the sample size was reduced to 517 patients (ASA; n=322, N-ASA; n=195). The ASA group had significantly higher rates of patients above age 75; patients taking anticoagulants, statins or angiotensin converting enzyme inhibitors; and patients with a prior history of peripheral vascular disease (P<0.05). ASA patients were not more likely to have mitral or aortic valve surgery. On logistic regression analysis, no significant differences were found in the rate of postoperative complications, including 30-day mortality. However, a trend towards a decreased incidence of MACE and an increased incidence of renal failure and intra/postoperative blood transfusion was evident [Table 1].
Conclusion: In a propensity-matched cohort, preoperative aspirin use was not associated with an increased incidence of adverse events in patients undergoing combined CABG and valve procedures. These patients often comprise a distinct group since coronary disease is frequently found incidentally in valve surgical candidates. The utility of aspirin administration in the preoperative period in such patients deserves further evaluation.