R. K. Schmocker1, S. B. Reeder2, E. R. Winslow1, S. M. Weber1 1University Of Wisconsin,Surgery,Madison, WI, USA 2University Of Wisconsin,Radiology,Madison, WI, USA
Introduction: Cystic pancreatic tumors present a diagnostic dilemma, as initial imaging often fails to provide a definitive diagnosis; therefore serial imaging is needed to follow the lesion over time. CT scan has traditionally been used to follow these lesions, however, given its excellent depiction of fluid containing lesions, and its lack of ionizing radiation, MRI has been increasingly utilized to assess these lesions. We sought to evaluate an initial experience and costs utilizing a novel pancreatic cyst-specific protocol for MRI.
Methods: A single center retrospective study was performed by searching an electronic imaging database for MRI pancreas studies from 2006-2014. After identification of the studies, the reports were examined to confirm that the indication for imaging was pancreatic cystic lesions. Retrospective chart review was used to assess demographics, imaging profiles (presence of other serial imaging – ex: CT), and the presence of interventions. Reimbursed costs of the studies were determined using the CMS physician fee data for the imaging procedures including both the professional and technical components, however contrast cost was not included.
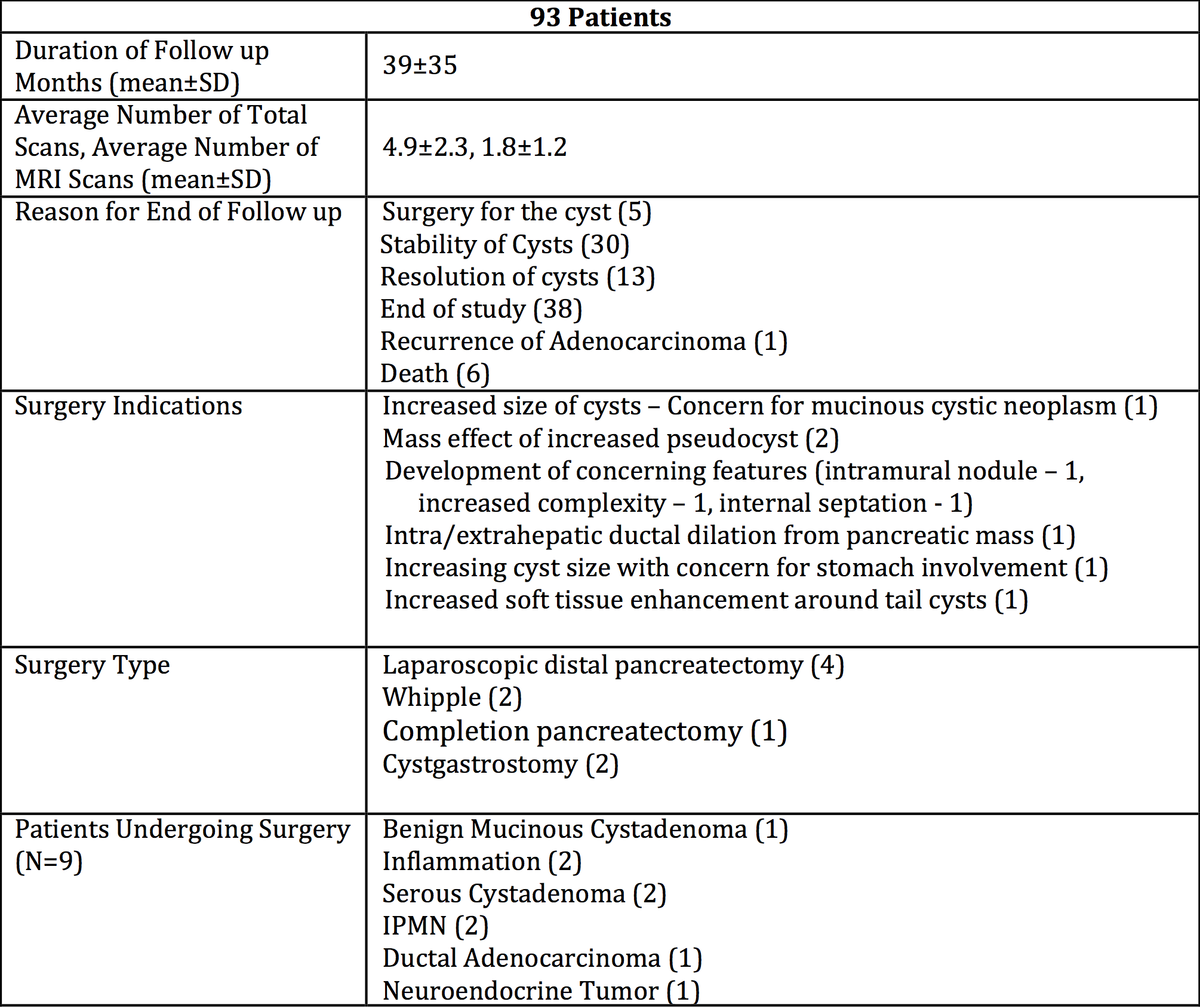
Results: 93 patients underwent an MRI pancreas protocol (average age: 65±13, % female: 61.5%). All patients had one contrasted imaging scan (MRI or CT) during the study period. 9 of these patients underwent a surgical intervention for a pancreatic cyst – 5 with a definitive operation, while 4 underwent surgery, but required surveillance of cysts in the remaining pancreas. Surgery was most often indicated due to concerning features or size (n=6). An MRI pancreas was used to diagnose cyst change for 3/5 patients that had a definitive operation, while CT scan identified a change in imaging characteristics for the other 2 patients. 43 patients underwent EUS/FNA during the study period. The average follow-up was 39 months, with the time between studies being 8.2 months. Patients had, on average, a total of 4.9 scans over the 39 months (1.7 CT scans, 1.3 MRI w/contrast, and 1.8 MRI pancreas protocol scans) or 1.5 scans per year. MRI pancreas was more expensive than CT w/Contrast ($333 vs. $230), but with the absence of radiation and contrast related complications. Additionally, if the average patient were exclusively followed with CT scans; the overall cost savings would be minimal ($189).
Conclusion: Our initial experience with the use of a novel pancreas protocol MRI is favorable, with minimal increase in cost. The lack of ionizing radiation and intravenous contrast with the MRI pancreas potocol, is an important consideration for patients undergoing serial imaging. The use of MRI for patients with pancreatic cystic disease shold be investigated further.