A. MacDonald1, K. P. Samy1, B. S. Parker1, T. Truong3, M. Kuchibatla3, J. Espinosa1, M. McRae1, J. Cheeseman1, A. D. Kirk1,2, T. V. Brennan1 1Duke University,Department Of Surgery,Durham, NC, USA 2Emory University,Department Of Surgery,Atlanta, GA, USA 3Duke University Medical Center,Biostatistics And Bioinformatics,Durham, NC, USA
Introduction:
Serum creatinine (sCr) remains the primary screening tool for renal transplant rejection, increasing only after significant damage has been done to the allograft. Acute injury-specific markers may provide an earlier and more sensitive measure of rejection. Urinary N-acetyl-beta-D-glucosaminidase (NAG) is produced in the nephron proximal tubules, which are injured during renal allograft rejection. We retrospectively analyzed urine samples from renal transplant patients to investigate its use as a biomarker for allograft rejection.
Methods:
We retrospectively analyzed 126 urine samples from renal transplant patients collected at two institutions for urinary NAG activity and Cr levels. Raw urinary NAG activity and NAG activity corrected for urinary Cr were correlated to clinical outcome. Analyses were run both with the raw NAG values and also corrected for urine concentration by dividing by the urine creatinine (corrected-NAG).
Results:
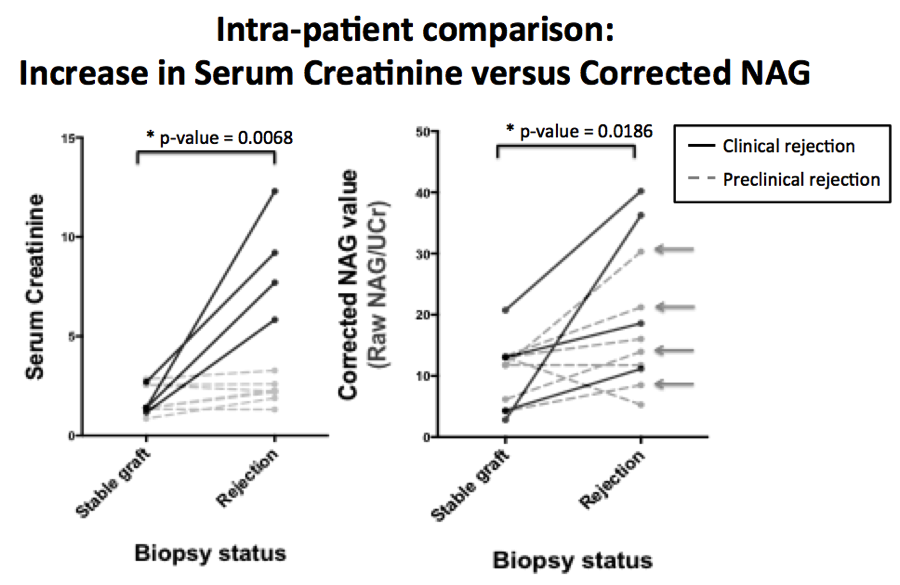
There was a statistically significant elevation in urinary NAG between healthy controls and transplant patients when samples were tested independently (raw NAG p=0.028, corrected-NAG p=0.003). There was a statistically significant increase from a patient’s baseline (during normal graft function) to periods of rejection within single patients for both raw NAG (p=0.002) and corrected-NAG (p=0.02) (Figure 1). Many patients with confirmed histological rejection on protocol biopsy had significant elevations in corrected NAG activity without elevation in sCr (Arrows, Figure 1). There was no significant difference between stable allograft and rejection NAG activity when testing independent samples (raw NAG p=0.143, corrected-NAG p=0.488). Elevations in NAG also occurred in the setting of BK nephropathy.
Conclusion:
Urinary NAG activity was associated with renal injury in transplant patients, with an acute elevation in NAG activity observed in the setting of biopsies showing rejection or BK nephropathy. However, it was not specific for acute rejection versus acute kidney injury from sources such as BK virus. Importantly, urinary NAG was elevated in patients without changes in sCr, indicating that it may serve as an earlier and more sensitive marker of kidney injury than sCr in the workup of a transplant patient.