S. Muralidharan1, T. Bodewes1, J. Johnson1, M. Auster1, M. Contreras1, F. W. LoGerfo1, L. Pradhan-Nabzdyk1 1Beth Israel Deaconess Medical Center,Vascular Surgery, Harvard Medical School,Boston, MA, USA
Introduction: The long-term success of vascular procedures is limited by the progression of intimal hyperplasia (IH) and subsequent loss of vessel patency. Injury at the time of implantation is known to result in dedifferentiation of vascular smooth muscle cells (VSMC) and inflammation contributing to IH; however, there is no current effective treatment that combats IH progression. Studies from our group have successfully demonstrated knock-down of IH-associated proteins, Thrombospondin-2 (TSP-2) and Myristoylated Alanine-Rich C-Kinase Substrate (MARCKS) using siRNA in a rat model of vascular injury. The present study evaluates Transforming Growth Factor-beta (TGF-) expression and macrophage infiltration, the known effectors of IH following siRNA treatment.
Methods: One of the common carotid arteries (CCAs) was denuded in Wistar rats, using a 2F Fogarty balloon catheter. Following denudation, the artery was transfected intraluminally for 15 minutes with one of the following treatments: saline, transfection reagent Polyethylenimine (PEI), or PEI + siRNA(s) (non-targeting, siTSP-2, siMARCKS, or siTSP-2 + siMARCKS) (n=4). The denuded and non-denuded arteries were harvested at 21 days. Immunohistochemical analysis was performed to evaluate TGF- protein expression and macrophage infiltration, as well as phenotype polarization. TGF- protein expression is presented as an arbitrary score (1 to 5). Total macrophage infiltration was determined by counting all CD68+ cells and polarization by measuring pro-inflammatory M1+ (CD68+/iNOS+) and anti-inflammatory, M2+ (CD68+/CD206+) macrophages and calculating the M1/M2 ratios.
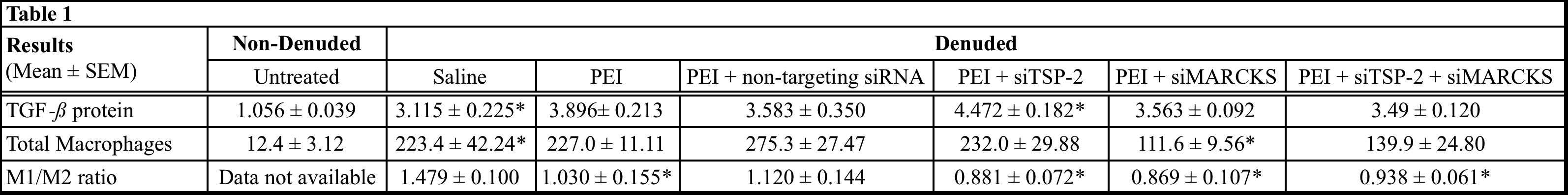
Results: Data are summarized in Table 1. Statistical significance was measured by comparing denuded saline group vs. non-denuded untreated group to validate the effect of arterial injury on TGF- expression and macrophage infiltration. For both TGF- expression and macrophage evaluation, to measure the effect of the treatment, data in the denuded treatment groups were compared to denuded saline group. Data are expressed as Mean ± SEM * = P < 0.05.
Conclusions: TSP-2 and MARCKS may play a role in modulating the macrophage polarization and their knock-down may ameliorate arterial injury-related inflammation thereby curtailing IH progression. Although the mechanism of MARCKS-mediated regulation of macrophages remains unclear, TSP-2 seems to be involved in the regulating expression of TGF-ß, a known modulator of the inflammatory response.