A. H. Siddiqui1, A. A. Javed3, S. Zafar2 1Aga Khan University Medical College,Medical College,Karachi, Sindh, Pakistan 2University Of Maryland,Department Of Surgery,Baltimore, MD, USA 3Johns Hopkins University School Of Medicine,Department Of Surgery,Baltimore, MD, USA
Introduction:
Cancer surgery is an essential component of healthcare. However, its availability is disparate around the world. Resource mobilization and advocacy requires better measurement of the burden of cancer surgery. We aimed to estimate the global need for cancer surgery and identify disparities by country income status.
Methods:
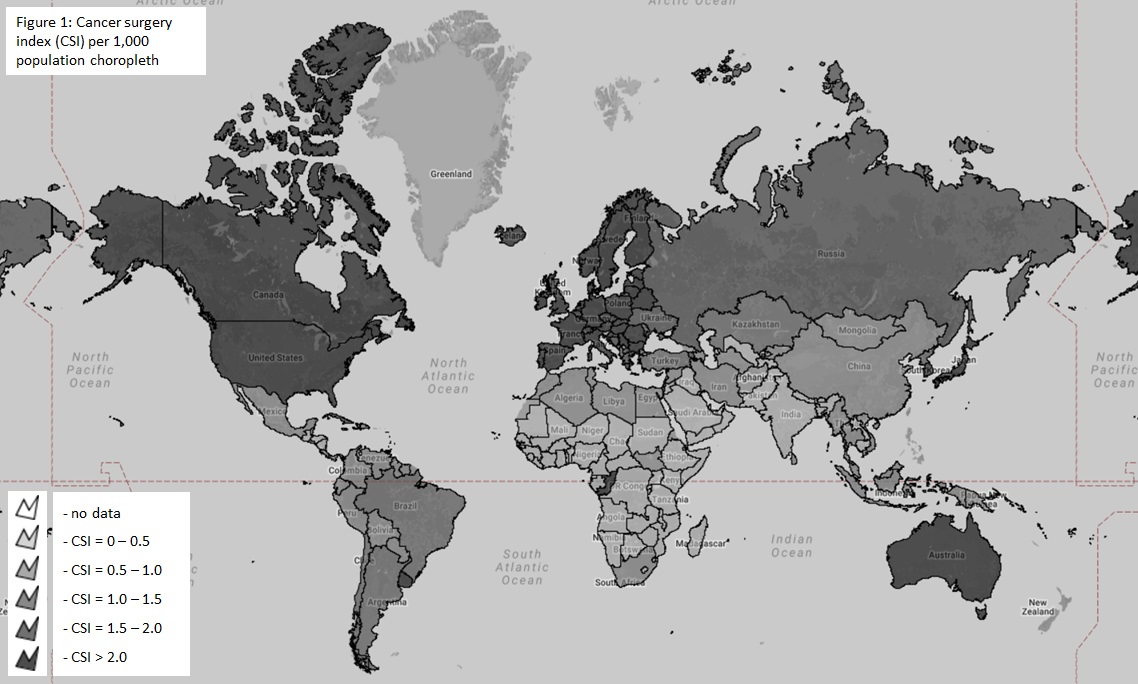
The WHO International Agency for Research on Cancer (IARC) and Global Cancer Observatory (GCO) were queried for data on the incidence of various malignancies in each country. As the incidence of cancer is dependent upon the ability to detect it we only estimate the ‘known’ need for cancer surgery. From the United States Surveillance, Epidemiology and End Result (SEER) database we extracted all patients with a new cancer diagnosis. The proportion of patients requiring surgery for each of these cancers was calculated. This was used to estimate the need for cancer surgery by multiplying with the incidence of each corresponding cancer in each country. The sum for each country was then divided by the population and multiplied by 1,000 to obtain a cancer surgery index (CSI). The Chi square test, t-tests, and Pearson coefficients were used to test associations between CSI and country income, national cancer policy, and presence of cancer registry. Results were tabulated and depicted as choropleth maps using eSpatial (Figure 1).
Results:
The number of people known to be in need of cancer surgery around the world in 2015 was 7,225,695 (± 9,524). The highest need was for breast cancer at 1.17 million patients requiring surgery followed by colorectal cancer (1.06 million). While low and lower-middle income countries make up 48% of the world’s population the reported cancer surgery need was only 21% of the global need highlighting disparities in detecting cancer in resource poor settings. The overall CSI was 0.99 per 1,000 population. The CSI varied almost linearly by income status, with the CSI being 1.95 per 1000 population for high income, 0.85 for upper middle income, 0.53 for lower middle income and 0.29 for low-income countries. Countries with national cancer policies and population based registries had higher CSIs (p<0.01). There was a significant positive relationship between a country’s human development index and the CSI (r=0.7, p<0.01).
Conclusion:
At least 7.2 million people around the world are known to require cancer surgery annually. Variations in the need for cancer surgery are related to a country’s income status, health care expenditure, availability of cancer data, and the presence of cancer control policies. There is an urgent need for systems strengthening in low and middle-income countries to ensure adequate access to cancer surgery.