S. R. Brown1, A. D. Person1, G. E. Mendoza1, M. Dale1, D. Rigg1, D. Keleny1, J. Dabestani1, D. K. Agrawal1, J. A. Asensio1 1Creighton University Medical Center,Surgery,Omaha, NE, USA
Introduction: The management of penetrating carotid artery injuries continues to evolve. Early questions regarding repair versus ligation have largely been settled in favor of repair for all but the most devastating injuries. To date, the use of temporary shunts to maintain cerebral perfusion in the repair of carotid artery injuries has not been well studied. Thus far, no single study has had the power to state whether the use of shunts makes any difference in neurological outcomes in the setting of penetrating carotid artery injuries.
Methods: A focused literature search was performed with PubMed, Scopus, and Ovid. PRISMA guidelines were followed. Inclusion criteria were those series reporting surgical repair for penetrating carotid artery injuries. Exclusion criteria were endovascular repair, neurosurgical techniques involving craniotomy, and studies with no reports on preoperative or postoperative neurologic status. Further relevant studies found as references in these papers were also evaluated. A total of 28 papers were identified that met these criteria, ranging from 1970 to 2012. Studies were systematically analyzed to extract cases of surgical repair for which both the utilization of temporary shunts and perioperative neurologic outcome data was reported. Non-parametric data was analyzed with Fisher Exact or Chi-Square tests as applicable. Statistical significance was set to a p-value less than 0.05.
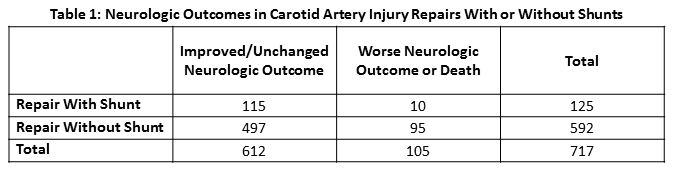
Results: There were a total of 717 carotid artery injuries. 592 were repaired without shunts. 125 were repaired with shunts. There was a trend towards lower overall mortality in repairs with shunts vs. those without shunts (5.6% vs. 9.8%; p=0.17). There was a trend towards increased rates of neurological improvement in repairs with shunts vs. those without shunts (13.6% vs. 10%, p=0.34). Patients undergoing repairs with shunts were more likely to have improved or unchanged neurologic outcomes in comparison to those without shunts (92% vs. 84%, p=0.018).
Conclusion: This focused analysis offers the first large scale evidence that the use of temporary shunts in the surgical repair of penetrating carotid artery injuries results in better neurologic outcomes in comparison to repair without the use of shunts. Based on this evidence, we recommend the routine use of temporary shunts during complex repair of penetrating carotid artery injuries.