D. R. Rigg1, A. Person1, M. Dale1, G. Mendoza1, S. Brown1, D. Keleny1, J. Dabestani1, D. Agrawal1, J. Asensio1 1Creighton University Medical Center,Department Of Trauma Surgery And Surgical Critical Care,Omaha, NE, USA
Introduction: Brachial vessel injuries remain uncommon, even in busy urban trauma centers, and therefore many trauma surgeons have limited experience with these types of injuries. Despite being a relatively uncommon injury, the brachial artery is the most frequently damaged artery in the upper extremity due to its vulnerability and close proximity to upper extremity bony structures. Therefore, trauma surgeons must be familiar with this injury and its associated outcomes. The objective of this study are: 1) review of the nationally reported experience with these injuries; 2) Identify predictors of outcome; 3) Compare predictors of outcome; 4) Report total charges incurred in the management of these injuries.
Methods: The National Trauma Data Bank (NTDB) was queried for pre-hospital admission data for brachial vessel injuries. Data extracted included demographics, vital signs on admission, and mechanism of injury. Univariate and stepwise logistics regression statistical analysis was used
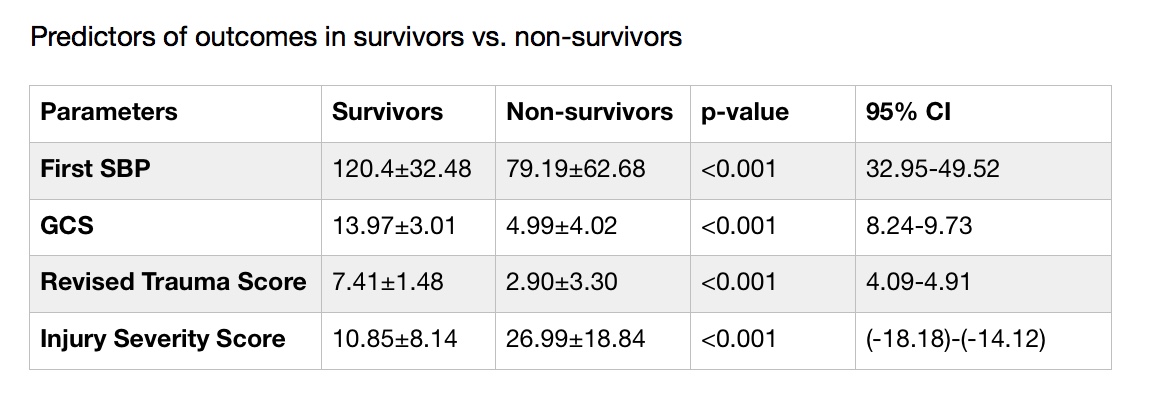
Results: There were 1,799 patients sustaining 1,900 brachial vessel injuries out of 1,466,887 patients registered in the NTDB from 2001 to 2005. Incidence was calculated to be 0.12%. Mean age at injury was 30 ± 14, mean RTS 7.23 ± 1.8, mean Glasgow Coma Scale 13.6 ± 3.5, mean ISS 11.5 ± 9.5. Mechanism of Injury: penetrating n=1,114 (61.9%), blunt n=699 (37.1%), and non-specific n=16 (1%). Mean initial SBP 119 ± 32.5; overall and adjusted survival rates: survivors 94.7%; non-survivors 5.3%. Patients underwent surgical repair n=671. Stratified as primary arteriorrhaphy 369 (55%), RSVG 165 (24.5%), resection of upper limb vessel with replacement 116 (17.3%), PTFE 21 (3.2%). Analysis revealed an increased ISS in the blunt injury group vs penetrating (10.65±8.82 vs 13.09±10.43; p<0.001). In survivors vs non-survivors, initial systolic blood pressure, glasgow coma scale, revised trauma score, and injury severity score were all statistically significant between the two groups (see table).
Conclusion: Brachial vessel injuries remain a low incidence injury as is shown in the NTDB. The injury severity score has a higher correlation with morbidity based on mechanism of injury. The overall cost of all brachial injuries was $22,954,998 in patient with extractable information (n=727).