K. M. Marsh1, A. Zhang1, D. Wu1, I. L. Kron2, Z. Yang1 1University Of Virginia,Surgery,Charlottesville, VA, USA 2University Of Arizona,Surgery,Tucson, AZ, USA
Introduction: We have identified a novel cardio-splenic axis that is activated and exacerbates myocardial infarct size (IS) during myocardial ischemia-reperfusion injury (IRI). HMGB1 and cell-free DNA (cfDNA) are released from ischemically-injured myocardium into the bloodstream during reperfusion. Facilitated by the interaction between HMGB1 and RAGE on splenic leukocytes, cfDNA enters the leukocytes, stimulates cytosolic TLR9 and augments inflammatory responses, ultimately exacerbating myocardial IS. Hydroxychloroquine (HCQ) is a well-known antimalarial agent and has recently been found to inhibit TLR7/9. We hypothesized that HCQ would attenuate myocardial IRI by inhibiting interferon I-mediated inflammatory responses.
Methods: Wild-type (WT) C57BL/6 and congenic TLR9-/- mice underwent 40 minutes of ischemia following treatment with TLR9 inhibitor ODN-2088, HCQ, or control 5 min prior to left coronary artery (LCA) occlusion. After 60 minutes of reperfusion, hearts were harvested and IS as a percentage of risk region (RR, % of LV) was measured by TTC-Phthalo blue staining. Ex vivo, isolated splenocytes were treated either with PBS or cardiac perfusate (CP) containing high levels of cfDNA and HMGB1 collected from hearts harvested after 40 minutes of LCA occlusion without reperfusion. Cell culture supernatant was then collected at 2 and 4 hours to measure IFNα and IFNβ.
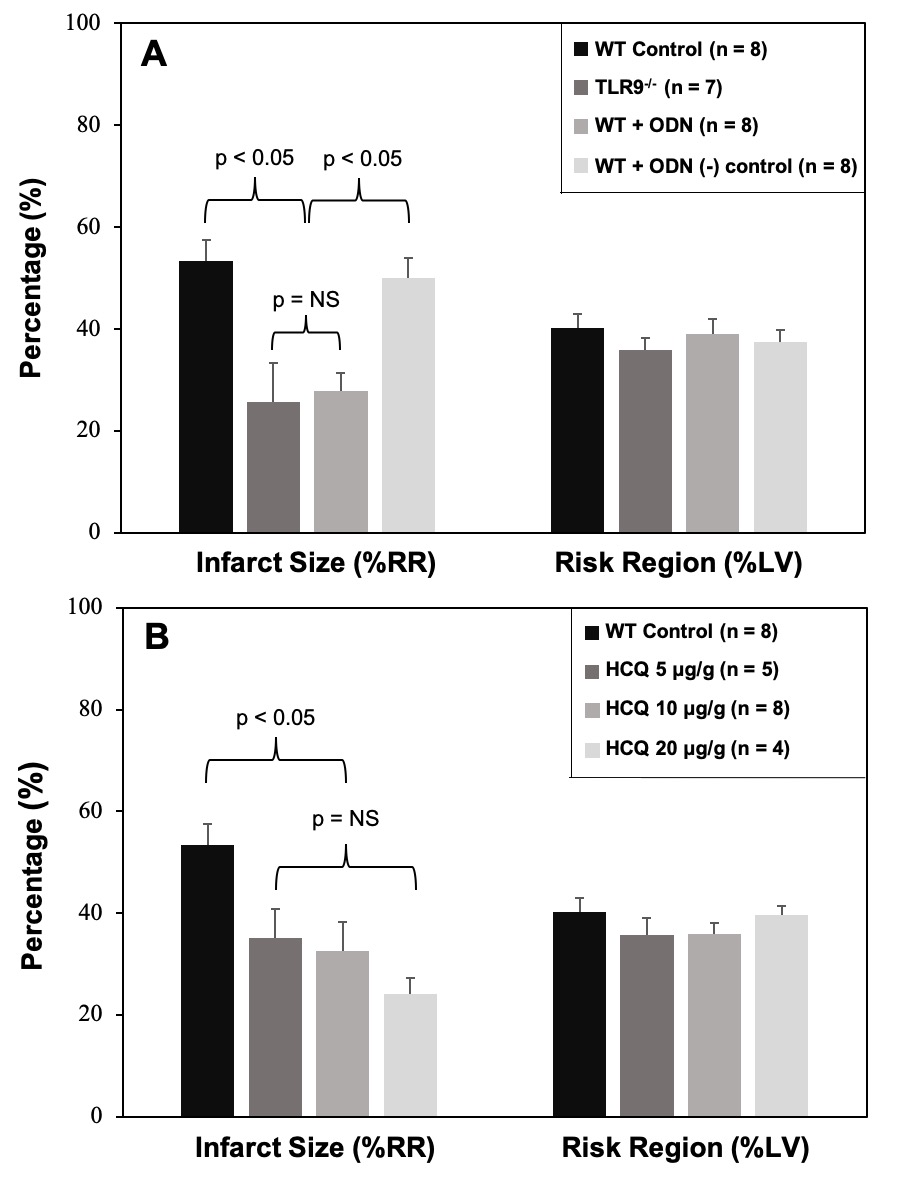
Results: In WT mice treated with ODN-2088, ODN negative control, or PBS control and TLR9-/- mice, there was no significant difference in RR (p=NS). In TLR9-/- mice and OND-2088-treated WT mice (0.6 μ g/g mouse weight), IS was significantly decreased to 26±8 & 28±4% respectively, a >49% reduction compared to WT mice treated with PBS (53±4%, p<0.05, Figure A). ODN-2088 negative control (0.6 μg/g) had no infarct-sparing effect (p=NS, vs. WT control). In WT mice treated with HCQ, RR was comparable among the control and 3 HCQ-treated groups. All 3 HCQ-treated mice (at dosages of 5, 10 and 20 μg/g) had significantly reduced IS (vs. WT control, p<0.05), with the 10 ug/g dose decreasing IS to 33±6% (39% reduction from WT control). A trend towards HCQ dose-response in IS reduction was present but did not reach statistical significance. (Figure B). In the ex vivo experiment, CP-treated splenocytes produced significantly higher IFNα and IFNβ in culture supernatant at 4 hours. HCQ significantly reduced the production of IFNα and IFNβ.
Conclusion: HMGB1 and cfDNA released from ischemic myocardium during reperfusion exacerbate myocardial IS by activating TLR9/IFN I-mediated inflammatory responses. Hydroxychloroquine reduces production of IFN I and attenuates myocardial IRI, likely via TLR9 inhibition.