N. Haywood1, A. Zhang1, E. Rotar1, S. Noona1, H. Ta1, M. Salmon1, I. L. Kron1, V. E. Laubach1 1University of Virginia Health System,Surgery,Charlottesville, VA, USA
Introduction: Ischemia-reperfusion (IR) injury after lung transplantation is a major cause of early graft dysfunction and increases the risk of early morbidity and mortality. Purinergic P2Y2 receptors (P2Y2R) are G-protein coupled receptors that are known to modulate the inflammatory response by enhancing inflammatory cell infiltration and activation. This study tests the hypothesis that P2Y2R modulates lung IR injury.
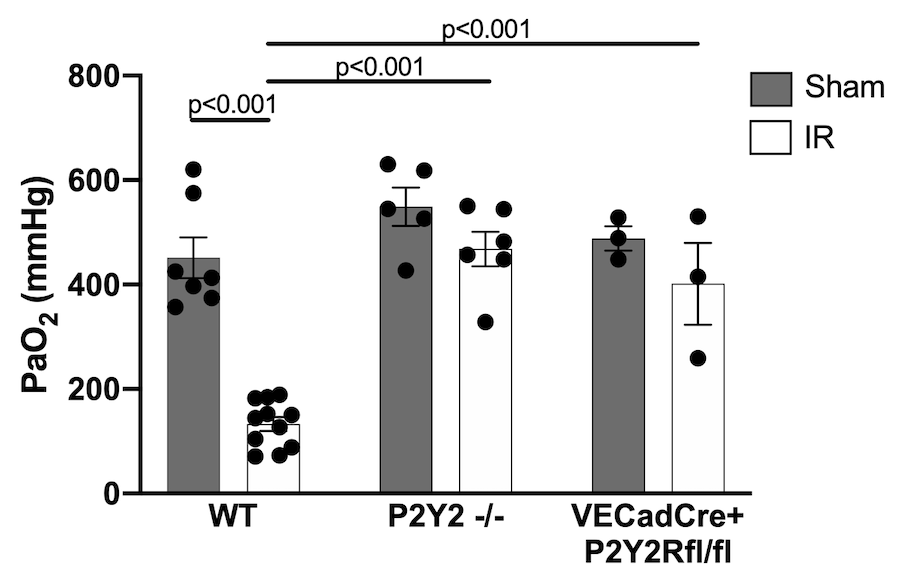
Methods: C57BL/6 wild-type (WT), P2Y2R-/-, and endothelial-specific P2Y2R (VECadCreP2Y2Rfl/fl) mice were subjected to lung IR or sham surgery using an in vivo left lung hilar-ligation model (1-hour ischemia, 2 hours reperfusion; n=3-11 mice/group). Left lung-specific partial pressure of oxygen (PaO2) was then measured to determine pulmonary function. Lung injury was assessed using wet-to-dry weight (WTD) ratio, and lung compliance was measured using a buffer-perfused isolated lung system. Murine lung primary microvascular endothelial cells (PMVEC) were exposed to hypoxia/reoxygenation (HR, 6 hours/4 hours) as a lung IR surrogate and treated with either P2Y2R inhibitor (AR-C 118925XX, 10µM) or vehicle to quantify the secretion of CXCL1 cytokine as an endothelial inflammatory marker. Data is presented as mean +/- SEM.
Results: Compared to WT, significantly improved oxygenation as measured by PaO2 following IR occurred in P2Y2R-/- mice (468.2±33.1 vs 133.1±13.2 mmHg, p<0.001) and in VECadCre+P2Y2Rfl/fl mice (401.3±78.6 vs 133.1±13.2 mmHg, p<0.001) (Figure). Similarly, a significant decrease in lung edema as measured by WTD ratio following IR occurred in P2Y2R-/- mice (4.86±0.15 vs 5.51±0.09, p=0.008) compared to WT. Lung compliance following IR was significantly improved in P2Y2R-/- mice (28.91±0.84 vs 14.86±0.83 µl/cm H2O, p<0.001) compared to WT. In vitro experiments using PMVECs showed a multifold increase in CXCL1 production following HR, which was mitigated with treatment of P2Y2R inhibitor (p=0.025).
Conclusion: Our results suggest that P2Y2R modulates the pulmonary inflammatory response following IR. This modulation is largely due to P2Y2R activity on pulmonary endothelium. P2Y2R may be a promising new therapeutic target to decrease the incidence of primary graft disfunction following lung transplantation.