R. Z. Strigenz1, P. B. Schwartz1, C. C. Stahl1, T. J. Aiken1, A. W. Acher1, E. H. Lawson2, D. Kravtsov1, P. R. Carney1, D. E. Abbott1 1University Of Wisconsin,Surgical Oncology,Madison, WI, USA 2University Of Wisconsin,Division Of Colorectal Surgery,Madison, WI, USA
Introduction: Patients living in geographically rural areas have increased barriers to healthcare access, including cancer care. Relative to urban populations, patients living in rural areas have an increased incidence of cancer and reduced survival, among other disparities. We sought to determine whether patient rurality was a driver of hospital cost for patients undergoing colectomy for colon cancer.
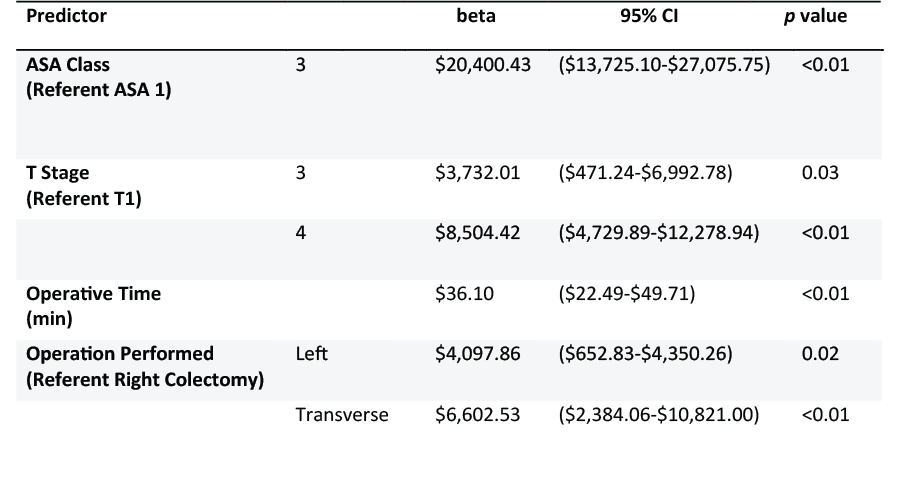
Methods: All patients undergoing colectomy for primary colon cancer at an academic medical center were queried from 2014 to 2019. Institutional cancer and cost accounting databases were combined, and patients were stratified into urban (1-3) and rural (4-10) cohorts by rural-urban commuting area (RUCA) codes. Bivariate analysis comparing the rural-urban cohorts and index hospitalization cost was conducted with student’s t-test, ANOVA, linear regression, and Kaplan Meier log rank analysis as appropriate. Relevant variables were entered into a multivariable linear regression to identify pertinent drivers of hospital cost. Significant variables on multivariable linear regression were reported as the beta (change in $ per unit change) with an associated 95% confidence interval.
Results:
279 urban and 142 rural patients were included in the final analysis. Rural patients were more likely to be non-Hispanic white (p=0.02), have lower alcohol use (p=0.03), differ in their insurance payor (p=0.02), undergo an open operation (p<0.01), be further from the treating institution (p<0.01), and have a worse median recurrence free survival (23.1 months vs. 27.1 months, p=0.04). On bivariate analysis, no differences in hospital cost was found between urban and rural patients ($12,151.16 vs. $13,082.61; p=0.42).
These findings were affirmed on multivariable linear regression analysis ($484.84; CI -1,699.69-2,637.38; p=0.67) after controlling for patient-related factors including age, race, rurality, insurer and ASA class, tumor-related factors including TNM staging and grade, and operative factors including operative time, open vs. laparoscopic procedure, and type of colectomy performed. Instead, on multivariable analysis (Table 1), statistically significant drivers of hospital cost included ASA class, T stage, operative time, and operation performed.
Conclusion: While differences between rural and urban patients undergoing surgical treatment for colon cancer exist, our results demonstrated no association between rurality and hospital cost. This persisted with multivariable analysis, suggesting that although patient rurality may affect various aspects of cancer care, institutions are able to provide the same high value care at costs similar to urban patients.