V. M. Welten1,2, K. Wanis3, A. C. Fields1, P. W. Lu1, R. A. Malizia1, J. Yoo1, J. E. Goldberg1, J. L. Irani1, R. Bleday1, N. Melnitchouk1,2 1Brigham And Women’s Hospital,Division Of General And GI Surgery, Department Of Surgery,Boston, MA, USA 2Brigham And Women’s Hospital,Center For Surgery And Public Health,Boston, MA, USA 3Harvard School Of Public Health,Department Of Epidemiology,Boston, MA, USA
Introduction: The management of rectal cancer has become progressively more complex, requiring a multi-disciplinary approach. Centralization of care has been increasingly discussed as a means to improve outcomes following high-risk cancer surgery. Prior studies assessing survival of patients with colorectal cancer have reported better outcomes when operations are performed at high-volume centers, with both lower complication rates and lower mortality rates, while others have suggested that differences in outcomes are related to degree of surgeon specialization rather than case volume. We aim to examine the association between facility volume and survival following proctectomy for rectal cancer.
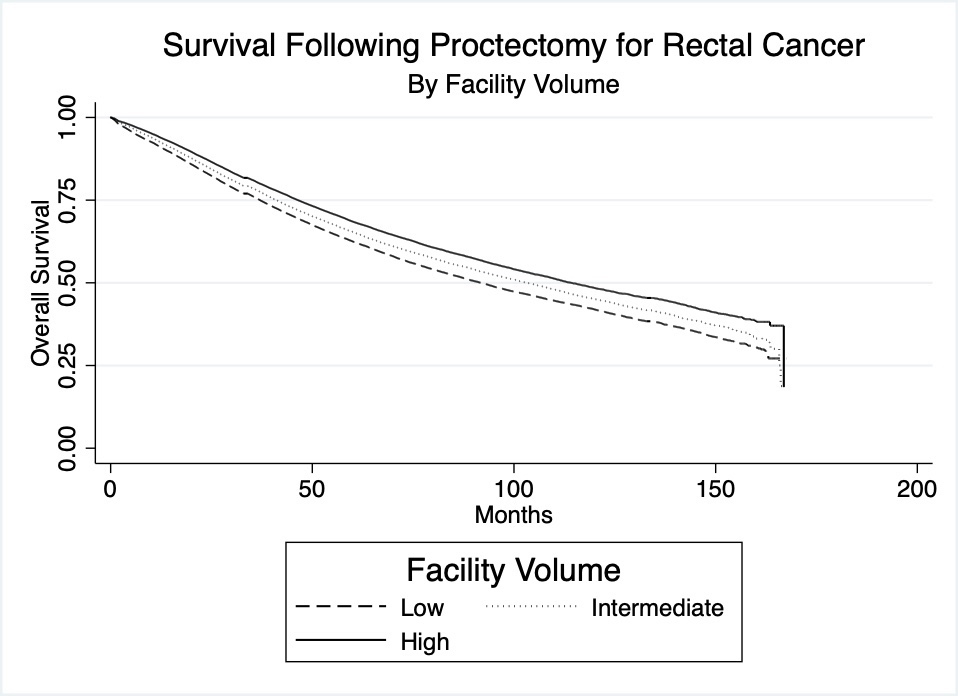
Methods: The National Cancer Database was used to identify all patients who underwent proctectomy for rectal cancer between 2004-2016. Facility volume was determined by the frequency of proctectomy for rectal cancer based on a facility’s unique ID, and was divided into tertiles – low, intermediate, and high. Median overall survival and 5-year survival for the patient cohort was compared between facility volume tertiles. Log-rank tests and Kaplan-Meier survival statistics were used for comparison.
Results: A total of 158,764 patients were included. Facilities were divided into low, intermediate, and high volume tertiles. When analyzing facility volume by facility type, for high volume facilities, 57% were academic and 38% were non-academic; for low volume facilities, 11% were academic, while 86% were non-academic (p<0.001). Median survival was 91.9 months (95%CI 90.1 – 93.5) for low volume facilities, 103.2 months (95%CI 101.3 – 105.5) for intermediate volume facilities, and 114.2 months (95%CI 111.9 – 116.7) for high volume facilities, with differences between tertiles statistically significant (p< 0.001). 5-year survival rates for the three tertiles were 62.5% (95%CI 62.0 – 63.0) for low volume, 65.4% (95%CI 64.9 – 65.8) for intermediate volume, and 68.5% (95%CI 68.1 – 69.0) for high volume (p<0.001). The corresponding Kaplan-Meier graph is presented in Figure 1: Overall survival following proctectomy for rectal cancer by facility volume.
Conclusion: This study identifies a strong association between facility volume tertile and survival following proctectomy for rectal cancer. Further work is needed to evaluate drivers of this association, whether there is a causal effect of facility volume on survival, and whether this relates to specialist expertise, compliance with treatment guidelines and delivery of standard of care, or other factors.