G. C. Linderman1, W. Lin2, M. Sanghvi1, R. D. Becher1, A. A. Maung1, B. Bhattacharya1, K. A. Davis1, K. M. Schuster1 1Yale University School Of Medicine,Surgery,New Haven, CT, USA 2Yale University,Statistics And Data Science,New Haven, CT, USA
Introduction: Laparoscopy is superior to open surgery for elective colectomy, but its role in emergency colectomy remains unclear. Previous studies were small and limited by confounding as surgeons may have selected lower risk patients for laparoscopy. We therefore studied the effect of attempting laparoscopy for emergency colectomies while adjusting for confounding using multiple techniques on large national databases.
Methods: Using National Surgical Quality Improvement Program data, we identified emergency colectomy cases from 2014 to 2018. We first compared outcomes between patients who underwent laparoscopic versus open surgery, while adjusting for baseline variables using both propensity scores with inverse probability of treatment weighting (IPTW) and regression. Next, we performed a negative control exposure analysis using the apparent benefit of laparoscopy in cases converted to open. By assuming that the group which converted to open did not benefit from the attempt at laparoscopy, we used the observed benefit to bound the effect of unmeasured confounding on our estimates. Finally, we analyzed the effect of laparoscopy in the National Inpatient Sample (2009-2011) using an instrumental variable (IV) analysis, with an instrument based on proportion of cases done laparoscopically at each institution.
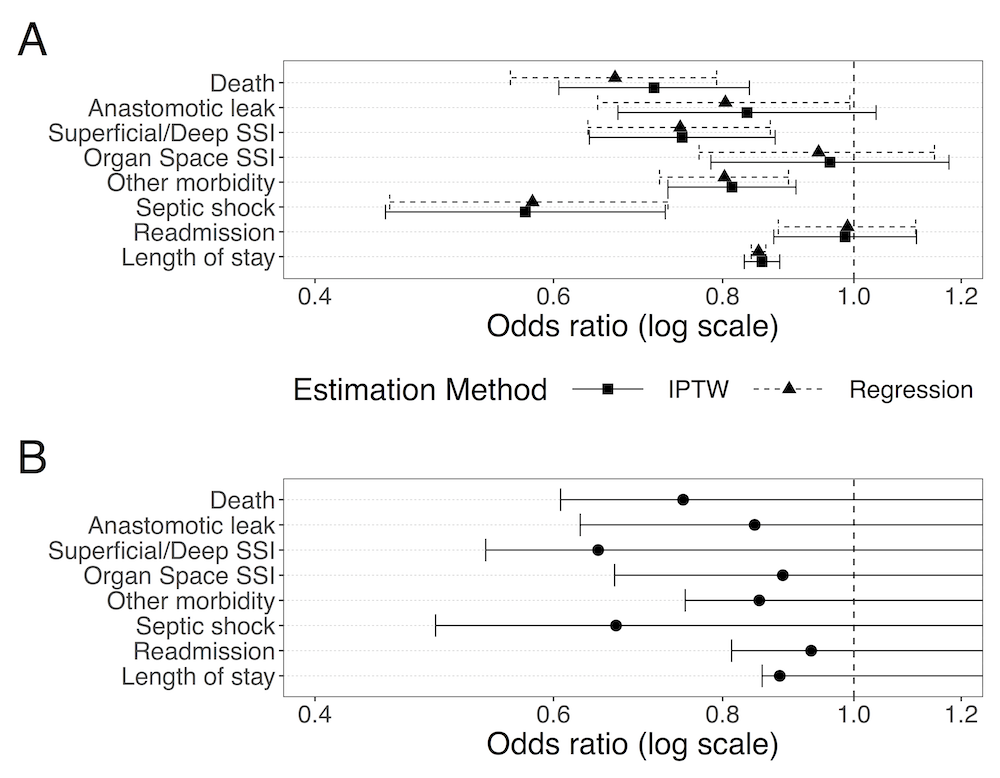
Results: Of 21,453 patients meeting criteria, 3,867 underwent laparoscopy, of which 1,375 converted to open. In both IPTW and regression analyses, attempting laparoscopy was associated with improved 30-day mortality, overall morbidity, anastomotic leak, surgical site infection (SSI), post-operative septic shock, and length of hospital stay (LOS) as compared to open surgery (Figure, Panel A). These effects do not appear to be driven by unmeasured confounding, as they were consistent with the lower bounds computed from the converted group (Figure, Panel B). IV analysis confirmed improved mortality and shorter LOS for laparoscopy.
Conclusions: Laparoscopic surgery for colorectal emergencies improves outcomes compared to open surgery. The benefit is observed even after adjusting for both measured and unmeasured confounding using multiple statistical approaches, thus suggesting a benefit not attributable to patient selection.