B. K. Roberts1, 3, C. Nofi1, 3, M. Kobritz1, 3, L. Demyan1, 4, M. Giangola1, 2 1Northwell Health, General Surgery, New Hyde Park, NY, USA 2Zucker School of Medicine at Hofstra, New Hyde Park, NY, USA 3Feinstein Institute for Medical Research at Northwell, New Hyde Park, NY, USA 4Cold Spring Harbor Laboratory, Cold Spring Harbor, NY, USA
Introduction: With growing accessibility, patients are increasingly relying on social media for medical information. However, social media sources vary in quality and accuracy of patient information. Thus, utilization of social media may lead to misinformation regarding treatment for patients in need of emergent general surgery procedures.
Methods: YouTube was searched with keywords “cholecystectomy,” “cholecystitis,” and “gallbladder surgery” as well as “appendectomy,” “appendicitis” and “appendix surgery.” For each general surgical procedure, the 100 videos with the greatest total views were chosen for review. Videos were assessed by four surgical trainees using two validated instruments: DISCERN, a measurement of the quality of health information, and the Patient Education Materials Assessment Tool (PEMAT), a measurement of understandability and actionability of patient education materials. A Likert scale was used to estimate the amount of patient education and misinformation. Chi-square test was used, and statistical significance was set at p<0.05.
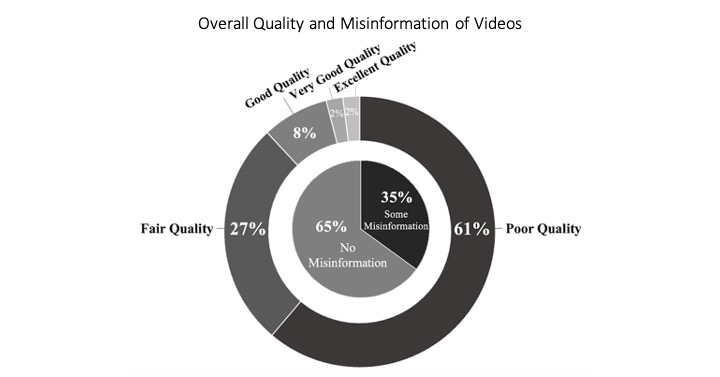
Results: The average number of views was 476,073 (93,670 to 7,976,292). The mean DISCERN score was 29.3 out of 75. The mean PEMAT scores were 64% for understandability and 22% for actionability. 49% of videos were rated as providing no patient education, while 29% provided some education and 22% provided a moderate level or more patient education. 35% of videos contained misinformation. The amount of misinformation was associated with type of video publisher; videos published by doctors, medical education and healthcare systems contained less misinformation, whereas videos published by patients, health/wellness groups contained more misinformation (p<0.001). Use of medical search terms “cholecystectomy” and “appendectomy” were associated with less misinformation (p<0.001, p=0.021). For counterpart colloquial searches, “gallbladder surgery” was associated with greater misinformation (p=0.001), whereas “appendix surgery” was not associated with misinformation.
Conclusions: There is a wide range of video quality that patients may use as resource for surgical information, with most videos being poor quality and providing little patient education. Although previous studies have shown that medical misinformation within social media exists, this study is the first to classify the scope of misinformation and quality of patient education related to emergency general surgery procedures. Understanding information available to patients online can help tailor surgeon-patient discussions to combat misinformation and improve the informed consent process for patients.