R. Howard1, Q. Solano1, L. Delaney1, B. Fry1, A. Ehlers1, M. Englesbe1, J. Dimick1, D. Telem1 1Michigan Medicine, Ann Arbor, MI, USA
Introduction: Use of mesh in clean/contaminated and contaminated ventral hernia repair (VHR) is controversial. While longitudinal trials have shown that mesh reduces long-term hernia recurrence, other studies have raised concern over increased infectious complications when mesh is placed in a contaminated field. The impact of this conflicting evidence on real-world mesh use is also poorly understood. We conducted the following study to understand current practice and outcomes in mesh use for clean/contaminated and contaminated VHR.
Methods: We performed a retrospective review of the Michigan Surgical Quality Collaborative Hernia Registry (MSQC-HR), which is a novel, statewide clinical registry that captures granular hernia-specific variables such as location and mesh use for patients undergoing VHR. The study cohort was adult patients undergoing clean/contaminated and contaminated VHR between January 1, 2020 and July 1, 2021. The exposure of interest was use of mesh which was classified as permanent or absorbable. The primary outcome was a composite end point of 30-day adverse events including complications, emergency department use, readmission, and reoperation. The secondary outcome was surgical site infection (SSI). Multivariable logistic regressions accounting for patient, hernia, and operative characteristics were estimated to calculate the independent association of mesh use with 30-day adverse events and SSI.
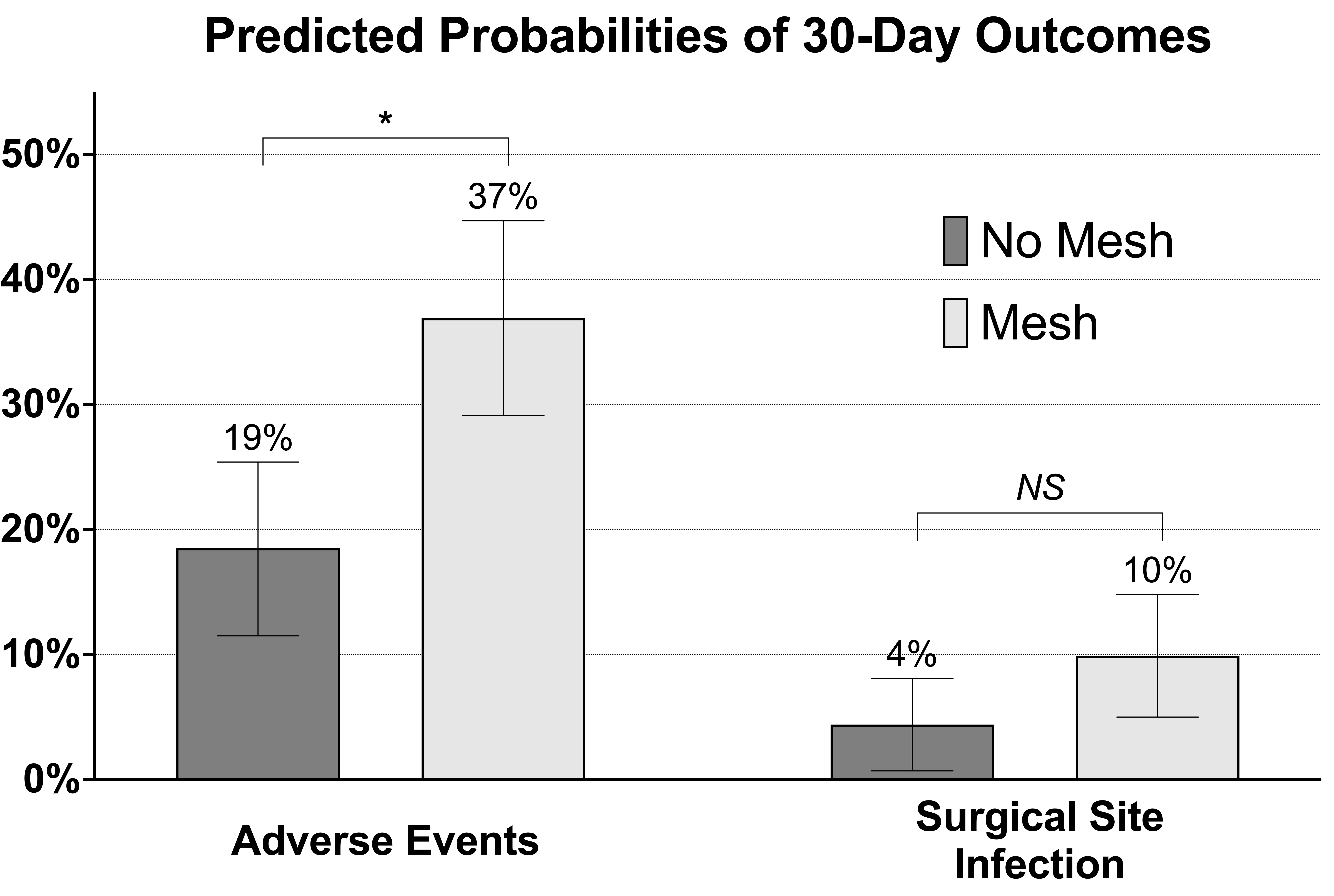
Results: 275 patients underwent clean/contaminated and contaminated VHR performed by 152 surgeons at 49 hospitals. Mean age was 56.4 (13.9) years and 152 (55.3%) patients were female. Mesh was implanted in 169 (61.5%) patients and consisted of permanent mesh in 147 (87.0%) patients and absorbable mesh in 22 (13.0%) patients. 30-day adverse events occurred in 57 (33.7%) patients with mesh and 23 (21.7%) patients without mesh (P=0.033), whereas surgical site infection occurred in 16 (9.5%) patients with mesh and 5 (4.7%) patients without mesh (P=0.149). After adjusting for patient, hernia, and operative characteristics, mesh use was associated with higher odds of adverse events after surgery (aOR 2.83 [95% CI 1.48-5.41]), but was not associated with higher odds of SSI (aOR 2.57 [95% CI 0.81-8.10]) (Figure).
Conclusion: In this study of real-world mesh use in clean/contaminated and contaminated VHR, mesh was used in most patients and was almost exclusively permanent. Although mesh placement was not associated with increased odds of infection, it was associated with increased adverse events even after controlling for patient, hernia, and operative characteristics. This suggests that additional work using granular hernia-specific data is needed to understand how mesh use drives adverse events after surgery in this population.