J. B. Oliver2, J. Rosado2, J. S. Patel2, K. M. Spiegler2, K. Houck3, R. J. Chokshi1 1New Jersey Medical School,Surgical Oncology,Newark, NJ, USA 2New Jersey Medical School,Surgery,Newark, NJ, USA 3New Jersey Medical School,Obstetrics And Gynecology,Newark, NJ, USA
Introduction: Cytoreduction surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) offer the best opportunity for long term survival for peritoneal metastasis for colorectal, appendicular, and ovarian cancers. Multiple studies have shown that individuals with cancer that are under insured have worse outcomes. However, to the best of our knowledge outcomes in the uninsured and underinsured undergoing CRS-HIPEC have not been investigated. Therefore, we looked at the outcomes in our series of CRS-HIPEC patients stratified by insurance status to see whether these individuals suffer worse outcomes.
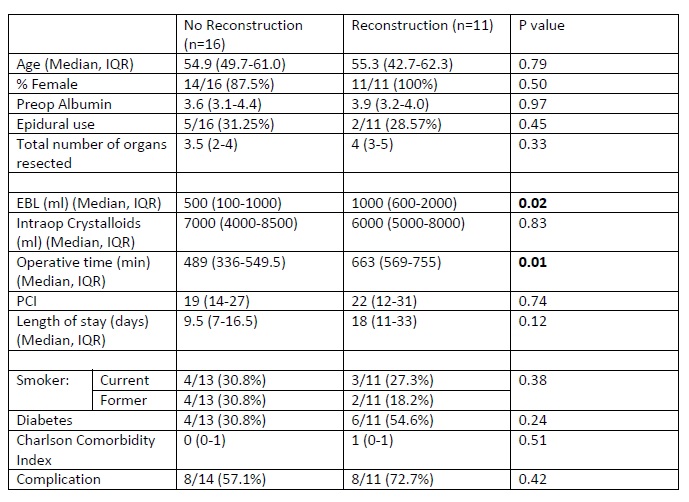
Methods: Demographics, comorbidities, intraoperative variables, and post-operative outcomes for all patients undergoing CRS/HIPEC at a single institution from 2012 to 2015 were analyzed. Variables were examined with chi squared or Wilcoxon Ranked Sum Test where appropriate. Survival was analyzed with Kaplan Meier curves and Cox Proportional Hazard Regressions.
Results:During this time frame, 27 individuals underwent CRS-HIPEC. Sixteen of these individuals were underinsured (either Charity Care or Medicaid) while 11 were insured (Medicare or private insurance). The median age of the underinsured group was significant lower than that of the insured group (54.1 years vs 62.3 years, p=0.02). The groups had similar distributions of the Charlson Comorbidity Index (0 vs 0, p=0.86) and peritoneal carcinoma index (25.5 vs 18, p=0.42). The under insured group had a higher preoperative albumin levels (4.0 vs 3.3, p=0.04). Both groups had similar distribution and total number of organs resected (3.5 vs 4 total organs, p=1.00). Operative time trended to being longer in the under insured group (573.5 minutes vs 510 minutes, p=0.06). Both groups had similar rate of major complications (Clavien Dindo complication of 3A or greater, 64.3% vs 63.6%, p=0.97) and length of stay (12 vs 11 days, p=0.98). Median follow up time for the under insured group was 8.5 months while the median follow up for the insured group was 1.7 months. During the follow up, 4 individuals in each group died; at 44, 71, 73, and 733 days within the under insured group the deaths occurred and at 16, 40, 41, and 72 days within the insured group. Survival was significantly better within the under insured group (p=0.02). After controlling for age and preoperative albumin, the survival difference remained significant improved within the under insured group (HR 0.02, 95% CI 0.00-0.76, p=0.04).
Conclusion:In this small, single center study with very short follow up, there was an improvement in survival for those underinsured undergoing CRS-HIPEC and no difference in length of stay or complications. Larger studies with longer follow up are needed to confirm these findings.